By – James M. Katz, BA
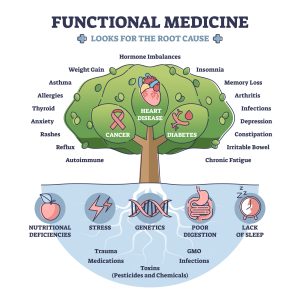
Holistic care in advanced practice nursing is transforming healthcare delivery, focusing on treating the whole person rather than just symptoms. This approach integrates physical, emotional, social, and spiritual aspects of health, leading to improved patient outcomes and satisfaction. Advanced practice nurses are uniquely positioned to implement holistic care strategies, combining their clinical expertise with a comprehensive understanding of patients’ needs and experiences.
The role of holistic care in advanced practice nursing encompasses various dimensions, including patient-centered care, integrative health practices, and wellness promotion. Certified holistic nurses and holistic nurse practitioners use holistic assessment techniques to gain a complete picture of their patients’ health status. This article will explore core competencies for holistic advanced practice nurses, evidence-based holistic interventions, and challenges in implementing holistic care across the lifespan. Additionally, it will discuss the future of holistic nursing practice and its potential to revolutionize healthcare delivery.
Holistic nurse practitioners, or HNPs, are specialized nurses who treat patients by looking at the whole person. They follow a philosophy that considers emotional, spiritual, and physical health. This way of thinking started with Florence Nightingale, who is seen as the founder of modern nursing. Holistic nursing is about creating balance and can be used in any healthcare setting.
Key Takeaways
- Holistic nursing looks at the whole person, not just the illness.
- Florence Nightingale started the idea of holistic nursing.
- Holistic nurses can work in any healthcare setting.
- They use different methods like mind-body practices and energy therapies.
- Holistic nurses need special training and certification.
 The Philosophy and Principles of Holistic Nursing
The Philosophy and Principles of Holistic Nursing
Historical Foundations
Holistic nursing has deep roots, tracing back to ancient healing traditions that viewed health as a balance of mind, body, and spirit. Over time, these ideas evolved, integrating with modern medical practices to form a comprehensive approach to patient care. Holistic nursing emphasizes the interconnectedness of all aspects of a person’s well-being.
Core Principles
At its core, holistic nursing is built on the belief that treating the whole person leads to better health outcomes. This philosophy includes not only physical care but also emotional, mental, and spiritual support. Nurses in this field use their knowledge, intuition, and compassion to create healing environments. They also prioritize self-care, understanding that a well-cared-for nurse can provide the best care to others.
Modern Interpretations
Today, holistic nursing continues to evolve, incorporating new research and techniques while staying true to its foundational principles. Modern holistic nurses work in various settings, from hospitals to private practices, always aiming to partner with patients on their journey to health. They respect each patient’s unique needs and cultural backgrounds, ensuring that care plans are personalized and effective.
The Role of Holistic Nurse Practitioners
Scope of Practice
Holistic nurse practitioners (HNPs) are advanced practice registered nurses who treat patients using a holistic approach. They focus on the whole person, not just specific symptoms or conditions. Their practice includes assessing physical, emotional, and spiritual health to identify imbalances and guide patients towards wellness. HNPs blend conventional medical treatments with holistic interventions to create a balanced care plan.
Key Responsibilities
HNPs excel in active listening, empathy, and building therapeutic relationships. They are skilled in recognizing both physical and emotional cues, which helps them provide comprehensive care. Their responsibilities include developing individualized care plans, educating patients on lifestyle changes, and using holistic therapies to promote overall well-being.
Interdisciplinary Collaboration
Holistic nurse practitioners often work with other healthcare professionals to ensure a well-rounded approach to patient care. They collaborate with doctors, therapists, and other specialists to create integrated treatment plans. This teamwork helps in addressing all aspects of a patient’s health, ensuring they receive the best possible care.
Defining Holistic Care in Advanced Practice Nursing
Holistic care in advanced practice nursing is an approach that addresses the patient’s physical, emotional, social, and spiritual needs, aiming to enhance overall well-being and quality of life rather than merely treating illness. This comprehensive method recognizes the interconnectedness of the bio-psycho-social-spiritual dimensions of a person, acknowledging that the whole is greater than the sum of its parts.
Principles of Holistic Care
The core principles of holistic care, as outlined by the Academy of Integrative Health and Medicine (AIHM), emphasize prevention, integration of healing systems, relationship-centered care, and individualized treatment . These principles guide advanced practice nurses in delivering care that is:
1. Compassionate: Holistic nurses are attentive, present, and empathetic towards patients.
2. Comprehensive: They treat the entire person rather than focusing on a single symptom.
3. Curious: Holistic nurses consider various factors affecting health, including environmental influences and dietary choices.
Integrating Mind, Body, and Spirit
Holistic nursing recognizes the body’s innate healing and restorative capacities. This approach extends beyond physical well-being to include emotional, social, and financial aspects of a patient’s situation. Advanced practice nurses practicing holistic care understand that positive emotions can enhance immune system functioning, diminish the inflammatory response to stress, and positively impact brain function. To integrate mind, body, and spirit effectively, holistic nurses draw on nursing knowledge, theories, research, expertise, intuition, and creativity. They honor the individual’s subjective experience about health, health beliefs, and values, becoming therapeutic partners with individuals, families, and communities.
Mind-Body Practices
Holistic nurses use mind-body practices to help patients connect their thoughts and feelings with their physical health. Techniques like meditation and guided imagery are common. These practices aim to reduce stress and promote relaxation, which can improve overall well-being.
Energy-Based Therapies
Energy-based therapies focus on the body’s energy fields. Methods such as Reiki and therapeutic touch are used to balance energy and promote healing. These therapies are believed to help with pain management and emotional health.
Integrative Approaches
Integrative approaches combine traditional Western medicine with alternative therapies. This can include nutritional counseling, exercise programs, and herbal remedies. The goal is to treat the whole person, not just the symptoms, for a more comprehensive approach to health.
Patient-Centered Approach
A patient-centered approach is fundamental to holistic care in advanced practice nursing. This model encourages active collaboration and shared decision-making between patients, families, caregivers, and providers. Patient-centered care has been defined as “Health care that establishes a partnership among practitioners, patients, and their families… to ensure that decisions respect patients’ wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care”.
Key elements of patient-centered care include:
1. Respecting patients’ values, preferences, and expressed needs
2. Coordinating and integrating care
3. Providing information, communication, and education
4. Ensuring physical comfort
5. Offering emotional support and alleviating fear and anxiety
6. Involving family and friends
7. Ensuring continuity and transition
8. Facilitating access to care
By implementing these principles, advanced practice nurses can create a healing environment that supports the whole person, fostering better health outcomes and patient satisfaction.
Core Competencies for Holistic Advanced Practice Nurses
Advanced practice nurses (APNs) who specialize in holistic care possess a unique set of competencies that enable them to provide comprehensive, patient-centered healthcare. These competencies encompass a wide range of skills and knowledge that allow APNs to address the physical, emotional, social, and spiritual aspects of their patients’ health.
Advanced Health Assessment Skills
Holistic APNs excel in conducting thorough and comprehensive health assessments. They partner with clients to explore and validate their stories, find meaning in their statements, and investigate contextual issues. This approach allows for a deeper understanding of the patient’s overall health status and life circumstances.
Key aspects of advanced health assessment skills include:
1. Assessing the effects of relationships and interactions among the client, significant others, and the community on the client’s well-being.
2. Using multiple sources of knowledge to understand the client’s needs and problems.
3. Interpreting diagnostic tests and procedures.
4. Assessing the client’s sense of coherence.
5. Utilizing esthetic interpretation and experiential knowing as sources of data collection.
These advanced assessment skills enable holistic APNs to gather a more complete picture of their patients’ health, considering not just the presenting symptoms but also the broader context of their lives.
Integrative Treatment Planning
Holistic APNs are skilled in developing comprehensive, integrative treatment plans that address all aspects of a patient’s health. They combine conventional healthcare treatments with holistic and integrative health practices to create personalized care plans.
Key elements of integrative treatment planning include:
1. Partnering with clients and other healthcare providers to formulate inter-professional outcomes.
2. Considering the relations among cost, risks, and benefits of the care plan.
3. Evaluating system-wide resources needed to carry out the holistic plan.
4. Collaborating with nurses and inter-professional teams to integrate resources for optimal holistic care.
5. Maintaining a dynamic assessment-diagnosis-outcome-implementation process to ensure holistic practice effectiveness.
Holistic APNs also provide patients with appropriate information about both conventional and integrative health practices, including potential side effects and costs. This approach empowers patients to make informed decisions about their care and actively participate in their treatment process.
 Therapeutic Use of Self
Therapeutic Use of Self
The therapeutic use of self is a crucial competency for holistic APNs. This involves using one’s personality, knowledge, and skills consciously to establish a therapeutic relationship with patients. The ability to engage in this type of relationship depends on the nurse’s personal and professional development.
Key aspects of the therapeutic use of self-include:
1. Developing self-awareness and engaging in self-reflection.
2. Integrating self-care and self-healing practices into their own lives.
3. Practicing mindfulness to enhance resilience and mental clarity.
4. Reconciling the ideal professional self with the actual professional self.
5. Cultivating empathy and building strong relationships with patients.
By developing these competencies, holistic APNs can create a healing environment that supports the whole person, fostering better health outcomes and patient satisfaction. Their unique emphasis on individually and holistically promoting health and well-being has resulted in APNs being the preferred healthcare providers for millions of patients worldwide.
Holistic Care Modalities in Advanced Practice
Advanced practice nurses employ a variety of holistic care modalities to address the physical, emotional, and spiritual needs of their patients. These modalities complement traditional medical treatments and reflect a commitment to treating the whole person.
Challenges and Opportunities in Holistic Nursing
Regulatory Issues
Holistic nursing faces several regulatory challenges. Different states have varying rules, making it hard for nurses to practice uniformly. Navigating these regulations can be tough, but it also opens doors for advocacy and policy change.
Public Perception
Public perception of holistic nursing is mixed. Some people see it as essential, while others are skeptical. This mixed view can be a hurdle, but it also offers a chance to educate the public about its benefits.
Future Trends
The future of holistic nursing looks promising. With growing interest in wellness and integrative care, holistic nursing is set to expand. This growth brings both challenges and opportunities for those in the field.
Mind-Body Techniques
Mind-body interventions focus on the interactions among the brain, body, mind, and behavior to promote overall health. These techniques include:
1. Meditation: Adapted from traditional Eastern systems, meditation enhances mental awareness and clarity. Mindfulness-based stress reduction (MBSR), a form of meditation, has shown promise in oncology settings.
2. Relaxation Therapies: These techniques aim to produce a state of mental and physical relaxation. They may incorporate deep breathing, guided imagery, progressive relaxation, yoga, self-hypnosis, and biofeedback.
3. Cognitive-Behavioral Therapy (CBT): Developed by Aaron Beck in the 1960s, CBT helps patients recognize and control their responses to symptoms through programmed education or counseling.
4. Hypnosis: This technique involves suggestions for changes in sensation, perception, cognition, affect, mood, or behavior within a therapeutic relationship.
5. Biofeedback: This process enables individuals to learn how to change physiologic activity to improve health and performance.
Nutritional and Herbal Therapies
Herbal medicine has been a cornerstone of healthcare for centuries, offering a rich source of bioactive compounds. https://aihcp.net/2024/06/13/role-of-holstic-nursing/ These treatments have been traditionally used for a wide range of conditions, including digestive disorders, respiratory ailments, and chronic pain. Advanced practice nurses may incorporate nutritional and herbal therapies as part of a holistic treatment plan, always considering potential interactions with conventional medications.
Energy Healing Practices
Energy healing practices are based on the belief that energy is vital and affects all body systems, impacting health and disease . Some common energy healing modalities include:
1. Therapeutic Touch (TT): A technique involving the practitioner moving their hands over the patient’s body to assess and manipulate their energy field.
2. Healing Touch (HT): Similar to TT, HT aims to restore balance in the patient’s energy system.
3. Reiki: An ancient healing method involving the laying on of hands to direct healing energy to various parts of the body. Reiki is thought to strengthen the immune system, restore vital energy, and ease various physical and emotional conditions.
4. Aromatherapy: The use of essential oils for therapeutic purposes. Anecdotal evidence supports its use in clinical settings to decrease pain and promote sleep.
These holistic care modalities are gradually being incorporated into clinical settings, with nurses observing improvements in vital signs, decreased pain and anxiety, and overall increased well-being when patients have access to these therapies. Advanced practice nurses are ideally positioned to identify patients who may benefit from these holistic approaches and to integrate them into comprehensive care plans.
Evidence-Based Holistic Interventions
Research on holistic nursing outcomes
Holistic nursing care (HNC) has gained significant attention in recent years due to its potential to improve patient outcomes and overall healthcare quality. Studies have shown that HNC enhances patient satisfaction by improving the quality of care. Conversely, the absence of holistic care has been linked to increased treatment costs, longer hospital stays, and a higher risk of developing new complications.
The practice of holistic care has been found to be an effective way to prevent diseases and death, as well as improve the quality of health care provided to patients. This approach considers the physical, social, spiritual, emotional, and economic needs of the patient, as well as their response to illness and ability to meet self-care needs.
Integrating conventional and complementary therapies
The integration of complementary and alternative medicine (CAM) therapies with conventional medicine has become increasingly prevalent. Hospitals, health maintenance organizations (HMOs), and individual physicians are incorporating CAM therapies into their practices. In 1998, only 6 percent of hospitals reported offering CAM services, but by 2001, this number had more than doubled to 15 percent.
HMOs have also shown growing interest in offering CAM therapies. A survey conducted between November 1998 and January 1999 found that two-thirds of HMOs (67 percent) offered at least one form of alternative care, with chiropractic (65 percent) and acupuncture (31 percent) being the most common.
The integration of CAM and conventional medicine is driven by several factors:
1. Patient demand: 49 percent of hospitals cited patient demand as the primary motivation for offering CAM services.
2. Organizational mission: 24 percent of hospitals stated that offering these services reflected their organizational mission.
3. Physician interest: Doctors want to keep up with their patients’ growing interest in and use of CAM.
Measuring holistic care effectiveness
Measuring the effectiveness of holistic care is crucial to its continued integration into mainstream healthcare. Research has demonstrated several positive outcomes associated with holistic nursing interventions:
1. Improved quality of life: There is a direct relationship between quality of life and holistic care [3, 5].
2. Enhanced patient satisfaction: Holistic care respects human dignity and involves patients in decision-making, leading to increased satisfaction.
3. Increased self-awareness and self-confidence: Holistic care has been shown to improve patients’ self-awareness and self-confidence.
4. Better understanding of patient needs: Holistic care increases the depth of care providers’ understanding of patients and their needs.
5. Improved harmony: Holistic care enhances harmony between mind, body, emotions, and spirit in an ever-changing environment.
To effectively measure holistic care outcomes, healthcare institutions are implementing various approaches. For example, a Holistic Health Practice Program for nursing students in Macao demonstrated significant improvements in promoting holistic health, self-esteem, and self-efficacy among participants. This program included essential components of physical, psychosocial, and spiritual aspects of holistic health.
As the integration of CAM and conventional medicine continues to evolve, it is essential to develop robust measurement tools and conduct further research to validate the effectiveness of holistic care interventions. This will help ensure that the benefits of holistic care are fully realized and can be consistently replicated across various healthcare settings.
Holistic Care Across the Lifespan
Pediatric holistic care
In recent years, there has been a growing recognition of the importance of a holistic approach to pediatric care. This approach considers not only the physical health of the child but also their emotional and mental wellbeing. By addressing all these dimensions simultaneously, healthcare providers can create a more comprehensive understanding of the child’s overall health and tailor treatment plans accordingly.
A holistic approach to pediatric care emphasizes preventive measures and health education. By empowering parents and caregivers with knowledge about nutrition, hygiene, mental health, and safety practices, healthcare providers can reduce the incidence of certain illnesses and promote healthier lifestyles from an early age. This approach also acknowledges that a child’s health is influenced by their social and environmental context, including factors like family dynamics, socioeconomic status, and access to healthcare.
Complementary therapies, such as art therapy, music therapy, yoga, and mindfulness practices, can play a valuable role in promoting emotional and mental wellbeing. These therapies offer alternative avenues for expression, relaxation, and coping, which can be especially beneficial for children facing emotional or behavioral challenges.
The whole child approach uses collaborative care, including physical, behavioral, developmental, and environmental health. This integrated care model offers versatile solutions to the challenges facing children today. When primary and behavioral practitioners bring their skills together, they support the physical, mental, and social-emotional health of the child. It also makes it easier to detect early onset of behavioral health issues and family risk factors.
Adult and geriatric holistic approaches
As individuals age, their healthcare needs evolve, requiring a more comprehensive approach to maintain overall wellbeing. Holistic care for older adults involves fostering health for mind, body, and spirit. Those who work with older patients with chronic illnesses or geriatric-specific medical needs must understand the value of holistic care to best support the geriatric population.
Geriatric care, often referred to as gerontology, is a specialized field of healthcare focused on the unique needs and challenges of older adults. It’s provided by healthcare professionals with advanced training in geriatrics, such as geriatricians, gerontological nurse practitioners, and geriatric social workers. The primary goal of geriatric care is to optimize the overall health and quality of life for seniors.
Comprehensive health assessments are the foundation of geriatric care. These evaluations help identify any medical conditions, cognitive impairments, or emotional concerns that may require attention. Geriatric care professionals are well-versed in the complexities of medication management for seniors, ensuring that prescriptions are optimized for safety and effectiveness.
For seniors with chronic health conditions, geriatric care specialists create personalized care plans that address their specific needs and monitor their conditions over time. Cognitive health is also a crucial aspect of geriatric care, encompassing the assessment and management of cognitive health issues like dementia and Alzheimer’s disease.
Home care is a flexible and personalized form of assistance designed to help seniors with their daily activities and needs while allowing them to remain in their own homes. Home care providers offer non-medical support and companionship to enhance seniors’ quality of life, assisting with activities of daily living, mobility support, meal preparation, and medication reminders.
End-of-life holistic care
Palliative care aims to alleviate the suffering of patients with life-limiting illness while promoting their quality of life. Its holistic approach means that care plans are tailored to treat symptoms such as pain, fatigue, nausea, and difficulty breathing, as well as to address psychological issues like depression or anxiety.
Symptom management is a cornerstone of palliative care. The palliative team works tirelessly to manage symptoms that cause discomfort, pain, or diminish quality of life. All therapies and medications are tailored to the individual’s needs and wishes and reflect the mind-body connection.
Facing a serious illness can be emotionally taxing for both the patient and their loved ones. Palliative care provides support through counseling, helping individuals navigate their feelings, manage stress, and come to terms with their situation. Some of the best types of psychological support include cognitive behavioral therapy, relaxation techniques, and meditation.
For many, serious illness prompts deep spiritual reflection. Palliative care teams often include or have access to spiritual care providers who can support patients and families through these existential explorations, respecting a wide range of beliefs and practices. This can help individuals in the moment and provide insight when making end-of-life decisions.
Palliative care also recognizes the social aspects of dealing with a serious illness. Social workers within the palliative care team can assist with practical issues such as coordinating care, understanding medical forms, and navigating the healthcare system. They can also offer support for the broader social impacts on the family unit.
Holistic Nursing in Various Clinical Settings
Hospitals and Clinics
Holistic nursing can be practiced in hospitals and clinics, where nurses provide care that considers the whole person. This approach integrates the patient’s mind, body, and spirit into the healing process. Nurses work closely with other healthcare professionals to ensure comprehensive care.
Community Health
In community health settings, holistic nurses focus on preventive care and health education. They engage with community members to promote wellness and address health disparities. This setting allows nurses to build strong relationships with patients and understand their unique needs.
Private Practice
Holistic nurses in private practice offer personalized care plans tailored to individual patients. They often use a variety of holistic modalities, such as massage therapy, acupuncture, and nutritional counseling. This setting provides the flexibility to spend more time with each patient and develop a deeper understanding of their health concerns.
Patient-Centered Care in Holistic Nursing
Individualized Care Plans
In holistic nursing, every patient is seen as a unique individual with their own set of needs and preferences. Care plans are tailored specifically to each person, ensuring that their physical, emotional, and spiritual well-being are all addressed. This personalized approach helps in creating a more effective and compassionate care experience.
Cultural Sensitivity
Holistic nurses understand the importance of respecting and incorporating a patient’s cultural background into their care. By being culturally sensitive, nurses can build stronger relationships with their patients, fostering trust and better communication. This approach not only honors the patient’s heritage but also enhances the overall care process.
Patient Empowerment
Empowering patients is a key aspect of holistic nursing. Nurses encourage patients to take an active role in their own health and healing. By providing education and support, holistic nurses help patients make informed decisions about their care, leading to improved outcomes and greater satisfaction.
Challenges in Implementing Holistic Care
Barriers in Healthcare Systems
Implementing holistic care in healthcare systems faces several challenges. One of the primary obstacles is the shortage of nursing staff and the resulting heavy workload. Many nurses experience burnout due to non-standard nurse-to-patient ratios and overwork, which significantly hinders their ability to provide comprehensive care. The focus on routine tasks and physical problems often overshadows the importance of addressing patients’ emotional, spiritual, and social needs.
Another significant barrier is the lack of organizational support for holistic care practices. Some healthcare managers do not prioritize spiritual care or consider it outside the hospital’s mission. This is reflected in hospital accreditation metrics that often fail to include holistic care assessment. The management system’s emphasis on documentation rather than performance further complicates the implementation of holistic care approaches.
Education and Training Needs
The educational system plays a crucial role in preparing nurses for holistic care, but current curricula often fall short. More than 90% of nursing education focuses on patients’ physical problems, neglecting other aspects of holistic care. This imbalance in educational content leaves many nurses ill-equipped to address patients’ diverse needs comprehensively.
The lack of specialized training in holistic care approaches, particularly in spiritual care and effective communication, is a significant challenge. Many nurses do not fully understand the concept of spiritual care due to its absence in undergraduate curricula and nursing texts. Additionally, the teaching methods employed are often educator-centered, limiting students’ exposure to practical training in considering patients’ various needs.
Educators’ competence in holistic care also presents a challenge. Some educators have limited knowledge of the various aspects of patients’ needs and their effects on health recovery, focusing more on routine tasks rather than providing examples of comprehensive care.
Future Directions for Holistic Advanced Practice Nursing
Emerging Holistic Care Models
As the field of nursing continues to evolve, there is a notable shift towards holistic care that considers the overall well-being of patients. This trend acknowledges the close connection between physical and mental well-being and aims to address the mental health needs of patients alongside their physical health concerns. The American Nursing Association (ANA) defines holistic care as an integration of body, mind, emotion, spirit, sexual, cultural, social, energetic, and environmental principles and modalities to promote health, increase well-being, and actualize human potential. The goals of holistic nursing are centered around improving health, reducing suffering, and preventing illness. Holistic nurses focus on protecting, promoting, and optimizing health and wellness. They also strive to provide support to individuals in finding peace, comfort, and balance during times of illness. This approach has shown promising results, as holistic care leads to prevention of patients’ depression, improved physical conditions, decrease in the duration of hospitalization, and faster recovery.
Technology and Holistic Care
The integration of technology in holistic care is becoming increasingly important. Advanced practice nurses are surrounded by computerized equipment and systems that assist them in recording and accessing patient information, monitoring patients’ progress, and aiding with the caring and healing processes. These technological advancements have the potential to enhance the delivery of holistic care in several ways:
1. Data Collection and Analysis: The collection of patient and medical data over time enables nurses to utilize and analyze patient information that can be stored for current and future reference. This comprehensive data can be analyzed by doctors and nurses when considering changes to the way they currently administer healthcare to patients.
2. Patient Monitoring: Computerized equipment monitors patients’ progress and vital signs, sending out alerts and warnings, often in less time than it would take a nurse to manually identify a problem. These systems enable the prompt treatment of illnesses when time is of the essence, giving faster and more accurate diagnoses.
3. Telemedicine: With the advent of telemedicine technology, medical professionals are now able to consult with patients online and provide solutions to their problems.
Patients can be fitted with devices that monitor their condition and feed the information to their healthcare provider at a remote location.
However, it’s crucial to note that technology can never replace the human element in nursing. As far back as the 1800s, nurses were trained to take the ‘whole person’ into account when treating their patients – spiritually, mentally, and physically. The combination of advanced analytics with the experience, knowledge, and critical thinking skills of nurses would result in making better clinical reasoning and clinical decision-making, which improves patient care at lower costs.
Policy Implications
The shift towards holistic care models and the integration of technology in nursing practice have significant policy implications:
1. Education and Training: There is a need to reframe nursing education to incorporate technology and machine learning in the curriculum. This will ensure that future advanced practice nurses are equipped to work effectively with emerging technologies while maintaining a holistic approach to patient care.
2. Evidence-Based Practice (EBP): The trend in many hospitals, clinics, and nursing homes today is toward evidence-based practice. Based on a combination of extensive research into practices that have had positive outcomes, as well as input from experienced medical practitioners and nurses, and taking into account the patient’s preferences, EBP has been found to be a more effective option in the treatment of patients.
3. Interdisciplinary Collaboration: Policies should encourage the formation of interdisciplinary medical and therapeutic teams to provide holistic interventions. This approach creates a communication channel between various team members, such as surgeons, general practitioners, physiotherapists, and dietitians, ensuring comprehensive patient care.
4. Ethical Considerations: As technology becomes more integrated into nursing practice, policies must address ethical considerations related to patient privacy, data security, and the appropriate use of artificial intelligence in healthcare decision-making.
By addressing these policy implications, the healthcare system can better support the future of holistic advanced practice nursing, ensuring that it continues to evolve and adapt to meet the complex needs of patients in an increasingly technological world.
Conclusion
Holistic care in advanced practice nursing has a significant impact on healthcare delivery, offering a comprehensive approach to patient well-being. This article has explored the core principles, competencies, and modalities involved in holistic nursing, highlighting its effectiveness across different life stages. The integration of conventional and complementary therapies, along with the use of technology, is shaping the future of holistic care. These developments have the potential to improve patient outcomes and transform the healthcare landscape.
To move forward, addressing challenges in healthcare systems, education, and reimbursement is crucial to implement holistic carefully. The evolving role of advanced practice nurses in delivering holistic care requires ongoing support through policy changes, enhanced training programs, and recognition of their unique contributions. As the field continues to grow, the focus on treating the whole person – mind, body, and spirit – will likely become an essential part of healthcare delivery, leading to better patient experiences and improved overall health outcomes.
Becoming a certified Holistic Healthcare Nurse can be earned completely online. Our Holistic Care program consists of 5 online holistic healthcare courses based off competency exams. Once finished, a candidate would then submit the online holistic healthcare application and would then be certified in Holistic and Integrative Healthcare for a period of 4 years. For full information about our Holistic Nursing program, please visit our site here.
FAQs
- What is holistic nursing?
Holistic nursing is a way of treating patients where nurses look at the whole person, not just their physical health. This means they consider emotional, spiritual, and other factors too. - Who can practice holistic nursing?
Any registered nurse can practice holistic nursing. It doesn’t matter where they work or what kind of patients they see. - Where do holistic nurses work?
Holistic nurses can work in many places like hospitals, clinics, community health centers, and even private practice. - 1. What makes holistic care essential in the nursing field?
Holistic care is crucial because it enables nurses to provide comprehensive care that encompasses not just the physical aspects of health but also considers other important factors like spirituality, social well-being, and overall life circumstances. This approach ensures that all facets of a patient’s health are addressed, including the effectiveness of their medications. - Can you explain what advanced holistic nursing entails?
Advanced Holistic Nursing (AHN) involves specialized courses that focus on integrating various healing practices to enhance health and well-being. These practices include mind-body techniques, manipulative body methods, and energy-based therapies, all aimed at promoting holistic health. - What is the foundational concept behind holistic nursing practice?
Holistic nursing is founded on the understanding that a patient’s health is influenced by a combination of biological, social, psychological, and spiritual elements. These elements are interrelated and contribute to the individuality of each patient. Holistic nursing, therefore, emphasizes personalized care that caters to the diverse needs of individuals. - What holistic modalities are commonly used by advanced practice nurses?
Advanced practice nurses have access to a variety of holistic modalities to enhance patient care. These include stress management techniques, breathing exercises, meditation, acupuncture, hypnotherapy, and therapeutic massage. These techniques and therapies are employed to support the overall health and well-being of patients. - What are the main ideas behind holistic nursing?
The main ideas are treating the whole person, using different kinds of knowledge, and working together with patients to help them heal. - Do holistic nurses need special training?
Yes, holistic nurses often get extra training or certifications to learn how to use holistic methods in their practice. - Is holistic nursing recognized as a specialty?
Yes, since 2006, the American Nurses Association has recognized holistic nursing as a specialty practice.
Research Articles:
Holistic care for patients with severe coronavirus disease 2019: An expert consensus. Hui Wang, Et Al. International Journal of Nursing Sciences, Volume 7, Issue 2, 2020, Pages 128-134, ISSN 2352-0132,
Multidisciplinary and Holistic Models of Care for Patients With Dermatologic Disease and Psychosocial Comorbidity: A Systematic Review. Patel A, Jafferany M. JAMA Dermatol. 2020;156(6):686–694.
Effects of hospital-family holistic care model on the health outcome of patients with permanent enterostomy based on the theory of ‘Timing It Right’. Xi Zhang RN, MD, Rui Gao MD, Et Al. Journal of Clinical Nursing JCN, Volume 29, Issue13-14 July 2020, Pages 2196-2208
Holistic approach to care for patients with endometriosis. Molina, Andreaa; Et Al. Current Opinion in Obstetrics and Gynecology 36(4):p 266-272, August 2024.










 A critical aspect of the forensic nurse’s role is the collection and preservation of evidence. This process is meticulous and governed by strict protocols to ensure that the evidence can be used in legal proceedings. Forensic nurses are trained in the proper techniques for documenting injuries, collecting biological samples, and maintaining the chain of custody for all collected evidence. Their detailed attention to the process ensures that the evidence gathered can withstand rigorous scrutiny in court.
A critical aspect of the forensic nurse’s role is the collection and preservation of evidence. This process is meticulous and governed by strict protocols to ensure that the evidence can be used in legal proceedings. Forensic nurses are trained in the proper techniques for documenting injuries, collecting biological samples, and maintaining the chain of custody for all collected evidence. Their detailed attention to the process ensures that the evidence gathered can withstand rigorous scrutiny in court.






 Written by Harriet Turner.
Written by Harriet Turner.