By – James M. Katz, BA
In the evolving landscape of healthcare, the role of a Holistic Nursing Specialist has garnered significant attention, marking a shift towards integrative approaches that encompass physical, emotional, mental, and spiritual health. Holistic nursing, embedding the principles of complementary and alternative medicine alongside traditional medical practices, offers a unique and comprehensive care model. This approach not only addresses the immediate health concerns but also the underlying factors contributing to the patient’s overall well-being, thus resonating with a holistic philosophy. Understanding what is a holistic nurse and exploring the pathways of holistic nursing certification can provide invaluable insights into the fusion of conventional healthcare with holistic healing practices, empowering patients through personalized care and fostering a deeper connection between patient and practitioner.
This article delves into the core of holistic nursing practice, outlining the roles, responsibilities, educational requirements, and benefits that define a Holistic Nursing Specialist. From detailing how to become a holistic nurse to examining holistic care in advanced practice nursing, it provides a comprehensive roadmap for aspiring holistic nurses. Furthermore, it explores the work environments conducive to holistic nursing practice, highlighting how holistic nursing and spirituality, alongside a broad spectrum of holistic nursing care techniques, contribute to a well-rounded healthcare delivery system. Through a blend of narrative and analysis, readers will gain a thorough understanding of the holistic nurse certification process, the essential qualities of a holistic nurse practitioner, and the transformative impact of holistic nursing on patient care.
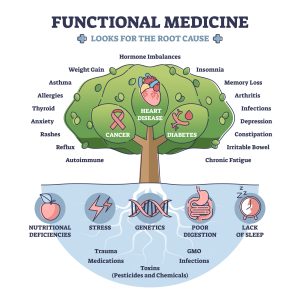
Holistic nursing is a unique field that focuses on treating the whole person, not just their physical symptoms. A holistic nursing specialist must consider the emotional, mental, spiritual, and environmental factors that affect a patient’s health. They use a mix of traditional nursing skills and alternative therapies to promote overall well-being. Recognized by the American Nurses Association since 2006, holistic nursing draws inspiration from the teachings of Florence Nightingale. This practice is applicable in various settings and benefits all types of patients.
Key Takeaways
- Holistic nursing treats the patient as a whole, considering mental, emotional, and spiritual health.
- The American Nurses Association recognized holistic nursing as a specialty in 2006.
- Holistic nurses use both traditional and alternative therapies to promote wellness.
- Education and certification are essential for becoming a holistic nurse.
- Holistic nursing can improve patient outcomes and provide professional fulfillment.
Defining Holistic Nursing
Holistic nursing is defined by the American Holistic Nurses’ Association as “all nursing practice that has healing the whole person as its goal”. This specialty is not just about the actions one performs but also embodies an attitude, a philosophy, and a way of being that requires nurses to integrate self-care, self-responsibility, spirituality, and reflection into their lives. Such integration often leads to a greater awareness of the interconnectedness of self, others, nature, spirit, and relationships within the global community.
Understanding Holistic Nursing
Holistic nursing is a type of nursing that cares for the whole person, not just their illness. It sees people as connected to their environment and focuses on healing and wholeness. Holistic nurses use their knowledge, skills, and intuition to help patients heal and grow. They work together with patients to create a healing process that fits each person’s unique needs.
Historical Background and Evolution
Holistic nursing has been around for a long time, but it has changed over the years. It started with the idea that caring for the whole person is important. Over time, it has grown to include new ideas and practices. Today, holistic nursing is used in many different places, like hospitals, clinics, and private practices.
Scope and Standards of Practice
Holistic nursing can be practiced anywhere, from hospitals to private clinics. It follows certain rules and standards to make sure patients get the best care. Holistic nurses believe that patients know their own needs best. They plan and provide care that respects each person’s culture, values, and beliefs.
The practice of holistic nursing is recognized by the American Nurses Association (ANA) as a distinct nursing specialty with clearly defined scope and standards. This recognition differentiates holistic nursing from general nursing practices, highlighting its unique contributions to health and healing. The specialty status helps in providing clarity to both nurses and the public, setting a foundational basis for holistic practices and amplifying the voice of the profession.
Daily Responsibilities
A holistic nursing specialist takes on many of the same tasks as regular nurses, but they do it with a different approach. They look at the whole person, not just the illness. They aim to remove barriers to healing and create a caring space for patients. This means they might use different methods to help people feel better, like talking about lifestyle changes or using natural remedies.
Skills and Competencies
Holistic nurses need a mix of regular nursing skills and special holistic skills. They must be good at listening and understanding what each patient needs. They also need to know about different healing methods, like mind-body practices and energy therapies. Being able to care for themselves is important too, because it helps them care better for others.
Work Environments
Holistic nurses can work in many places. They might be in hospitals, clinics, or even private practices. Some work in schools or community centers. Wherever they are, they bring a special focus on whole-person care. They help people find their best health by looking at all parts of their lives, not just their medical problems.
Holistic nursing encompasses various aspects of care, including physical, mental, emotional, spiritual, and environmental considerations. It views each person as a unitary whole, interacting continuously with the environment. This perspective acknowledges that the whole is greater than the sum of its parts. Holistic nursing specialists act as facilitators and instruments of healing, respecting the individual’s subjective health experiences, beliefs, and values. They engage with individuals, families, and communities to form therapeutic partnerships, utilizing a broad spectrum of nursing knowledge, theories, research, expertise, intuition, and creativity.
The practice of a holistic nursing specialist requires the integration of self-care, self-responsibility, spirituality, and reflection, which may lead to enhanced awareness of one’s interconnectedness with all aspects of life. This awareness is crucial for holistic nurses as it enhances their understanding of individuals and their relationships within the human and global community. Such understanding allows nurses to use their awareness to facilitate the healing process effectively.
Holistic nursing draws upon a unique body of knowledge, incorporating evidence-based research and sophisticated skills. The practice is supported by defined standards and a diversity of modalities from a broad spectrum of health practices. The holistic approach is grounded in a philosophy of living and being that emphasizes caring, relationship, and interconnectedness. Holistic nurses use these principles and modalities in their daily life and clinical practice to remove barriers to the healing process, creating a conducive space for healing while sharing their authenticity, caring presence, and nursing skills.
Overall, holistic nursing is a comprehensive practice that requires nurses to function across cognitive, experiential, and affective domains, utilizing knowledge, theory, expertise, intuition, and creativity to provide care that is truly holistic. This approach not only addresses the immediate health concerns but also the underlying factors contributing to the patient’s overall well-being, resonating deeply with holistic philosophy and enhancing the nurse-patient relationship.
Core Principles of Holistic Nursing Practice
Holistic nursing integrates a comprehensive view of patient care, emphasizing the interconnectedness of various health dimensions. This section explores the core principles that guide holistic nursing practice, focusing on unity and wellness, and the interrelationship between human beings and their environment.
Unity and Wellness
Florence Nightingale, often recognized as the founder of holistic nursing, emphasized unity and wellness as fundamental principles. Holistic nursing is defined by the American Holistic Nurses’ Association as a practice where “healing the whole person is the goal “. This involves treating individuals as complete units that function and interact within their environments, rather than addressing isolated symptoms or conditions.
Holistic nursing specialist incorporates self-care, self-responsibility, spirituality, and reflection into their practice, which fosters a greater awareness of the interconnectedness of self, others, nature, spirit, and the global community. This awareness enhances the nurse’s understanding of their patients and their relationships within the human and global community, allowing them to facilitate the healing process more effectively.
Interrelationship of Human Beings and Environment
The interplay between an individual’s health and their environment is a critical component of holistic nursing. Florence Nightingale’s legacy highlighted that our external environment significantly impacts health and wellbeing. She pioneered environmental considerations in nursing care, focusing on safe drinking water and the risks of atmospheric pollution in urban environments.
Today, holistic nursing specialists lead initiatives in healthcare by assessing the environments where people live, work, and play. They integrate environmental awareness, education, and preventive health strategies into their practice, improving health outcomes on both local and global levels. By understanding and addressing environmental factors, holistic nurses enhance patient care and contribute to healthier communities.
Holistic nursing practices are supported by a unique body of knowledge that includes evidence-based research and skills from both conventional healthcare and Complementary and Alternative Modalities (CAM). This integration allows holistic nurses to provide care that respects the patient’s physiological, mental, spiritual, and environmental conditions.
Mind-Body Practices
Holistic nurses often use mind-body practices to help patients manage stress and improve overall well-being. Techniques like meditation and breathing exercises are common. These practices aim to connect the mind and body, promoting relaxation and mental clarity. Guided imagery and cognitive therapy are also used to help patients visualize positive outcomes and reduce anxiety.
Energy-Based Therapies
Energy-based therapies focus on the body’s energy fields. Holistic nurses may use techniques like therapeutic touch and Reiki to balance energy and promote healing. These therapies are based on the idea that energy imbalances can lead to illness. By restoring balance, nurses help patients achieve better health. Aromatherapy, which uses essential oils, is another popular energy-based therapy.
Natural and Nutritional Approaches
Natural and nutritional approaches are also key in holistic nursing. Nurses may provide dietary coaching to help patients make healthier food choices. Herbal therapy is another common practice, using plants and herbs to treat various conditions. Exercise programs and hydrotherapy are also used to improve physical health and well-being.
In summary, the core principles of holistic nursing practice revolve around treating the patient as a whole entity, considering the intricate connections between their health and the environment. This approach not only addresses immediate health concerns but also the underlying factors contributing to the patient’s overall wellbeing. By embodying these principles, holistic nurses play a vital role in advancing health and healing within the broader context of their communities and the environment.
Roles of a Holistic Nursing Specialist
Healing the Whole Person
Holistic Nursing Specialists focus on healing the whole person, which is defined as all nursing practice aimed at treating the individual as a complete unit functioning within their environment. This approach involves assessing and integrating the physical, mental, emotional, spiritual, and environmental aspects of health. Holistic nurses utilize a variety of healing and integrative therapies, such as imagery, visualization, relaxation techniques, and stress management, to support patients in both hospital and private practice settings.
Self-Care Advocacy
Self-care is a fundamental aspect of holistic nursing, emphasizing the importance of nurses integrating self-care, self-responsibility, spirituality, and reflection into their lives. By advocating for self-care, Holistic Nursing Specialists not only enhance their own well-being but also set a standard of health and wellness that influences their patients and colleagues. Programs like the AHNA’s practice grant support the implementation of self-care routines among healthcare staff, promoting holistic health practices such as meditation, aromatherapy, and physical activities.
Environmental Stewardship
Holistic Nursing Specialists play a critical role in environmental stewardship within healthcare settings. They are often involved in Green Teams, which are committees focused on promoting sustainable practices and reducing the environmental impact of healthcare facilities. These teams, typically led by nurses, work on sustainability projects, spread awareness, and encourage staff participation to mitigate the healthcare industry’s environmental effects. Holistic nurses are equipped to educate and lead others in sustainable health practices, significantly impacting public health outcomes related to environmental sustainability.
Responsibilities in Holistic Nursing
Patient Education
Holistic Nursing Specialists prioritize patient education, focusing on the interconnectedness of health practices and personal wellness. They inform patients about the scope of conventional and non-conventional health care options, guiding them through the complexities of various health and healing professions, such as MDs, NDs, DCs, DOs, Lac’s, and LMTs. By providing comprehensive education, holistic nurses empower patients to coordinate their care effectively and make informed decisions about their health treatments.
Integrating CAM Therapies
Incorporating Complementary and Alternative Medicine (CAM) therapies into patient care is a key responsibility of a Holistic Nursing Specialist. They utilize a variety of CAM therapies including meditation, acupuncture, hypnotherapy, therapeutic massage, and herbal therapy to address the holistic needs of their patients . These practices are integrated thoughtfully to complement conventional medical treatments, ensuring a balanced approach to health and wellness. Holistic nurses are also responsible for maintaining their qualifications in these specialties to provide competent care within their practice.
Promoting Wellness
Holistic nurses are dedicated to promoting wellness by implementing integrative methods that focus on the patient’s overall health rather than just treating symptoms. This includes using non-pharmacological methods for pain control, encouraging self-care practices, incorporating spirituality into care plans, and promoting reflective practices among patients. By fostering a holistic approach to health, they help patients achieve a higher quality of life and prevent the recurrence of health issues. Holistic nurses also lead by example, adopting holistic principles and modalities in their own lives to enhance their effectiveness as caregivers and educators.
Educational Requirements
Required Education and Training
To become a holistic nurse, you need to start with a nursing degree, like an Associate’s or Bachelor’s in Nursing. After that, you can take extra courses in holistic health to learn more about natural and whole-person care. These courses help you understand how to treat the mind, body, and spirit.
Certification and Licensing
Once you finish your education, you can get certified by groups like the American Holistic Nurses Credentialing Corporation (AHNCC) or our organization the American Institute of Health Care Professionals (AIHCP). This certification shows that you know a lot about holistic nursing. You also need to have a nursing license to work as a nurse.
Continuing Education and Professional Development
Holistic nurses keep learning even after they start working. They go to workshops and take new courses to stay updated on the latest in holistic care. This helps them provide the best care to their patients and grow in their careers.
Benefits of Holistic Nursing
Patient Outcomes and Satisfaction
Holistic nursing focuses on treating the whole person, not just the symptoms. This approach often leads to better patient outcomes and higher satisfaction. Patients feel more understood and cared for, which can speed up their recovery and improve their overall well-being.
Professional Fulfillment
For nurses, practicing holistic care can be deeply rewarding. It allows them to connect with patients on a more personal level, making their work more meaningful. This sense of fulfillment can lead to greater job satisfaction and a longer, more satisfying career.
Community Impact
Holistic nursing doesn’t just benefit individual patients; it can also have a positive impact on the community. By promoting overall wellness and preventive care, holistic nurses help create healthier communities. This can lead to reduced healthcare costs and a better quality of life for everyone.
Work Environments for Holistic Nurses
Holistic nurses have diverse opportunities to practice in various healthcare settings, each offering unique challenges and benefits tailored to their holistic approach to patient care.
Hospitals and Clinics
In hospitals and clinics, holistic nurses often encounter a fast-paced environment where they assist patients with a variety of health conditions. Approximately 35% of holistic nurses work in acute care hospitals where their roles include nonpharmacological pain management and educating patients on stress management as part of recovery. These settings may require working at unconventional hours, including late nights, early mornings, or weekends, to accommodate patient care needs. Holistic nurses in these settings collaborate closely with other healthcare professionals to provide comprehensive care that addresses both medical and holistic health needs.
Private Practice
About 20% of holistic nurses operate in private practices. Here, they have more control over their schedules, often leading to a more predictable routine compared to those in 24-hour hospital settings. Private practice allows holistic nurses to delve deeper into specialized holistic modalities such as acupuncture, therapeutic massage, and meditation guidance. This setting enables them to build long-term relationships with patients, focusing extensively on holistic health strategies tailored to individual wellness goals.
Community Health Centers
Holistic nurses also contribute significantly in community health centers, where they play a crucial role in integrating community health with holistic practices. They work alongside other health professionals to address the broader health needs of the community, focusing on preventive care and holistic education. Nurses in these settings might also engage in public health initiatives, lead wellness programs, and provide holistic care across diverse populations, emphasizing the interconnectedness of health and environmental factors.
In each of these environments, holistic nurses bring a unique perspective to healthcare. They apply their knowledge and skills to enhance patient outcomes by treating the whole person—not just the symptoms—thereby supporting the overall well-being and long-term health of their patients. Holistic nurses are essential in bridging the gap between conventional medical treatments and holistic health practices, ensuring that patients receive a comprehensive, integrative approach to health care.
Benefits of Holistic Nursing
Holistic nursing offers a range of benefits that extend beyond traditional medical care, emphasizing a comprehensive approach to health that can profoundly impact both patients and nurses. This section explores the significant advantages of this practice, focusing on comprehensive patient care, professional fulfillment, and enhanced patient relationships.
Comprehensive Patient Care
Holistic Nursing Specialists provide care that encompasses not just the physical symptoms but also the psychological, social, and spiritual needs of patients. This all-encompassing approach ensures that all aspects of a patient’s well-being are addressed, which can lead to more effective treatment outcomes and improved patient satisfaction. By integrating Complementary and Alternative Medicine (CAM) therapies with conventional medicine, holistic nurses offer a diversified toolkit for patient care, allowing for tailored treatments that can better meet the individual needs of patients.
Professional Fulfillment
For nurses, the holistic approach offers a deeper sense of professional fulfillment as they engage in a practice that aligns with a nurturing, caring ethos. Holistic nursing allows practitioners to use their full range of skills and knowledge, fostering a sense of competence and pride. This comprehensive approach not only enhances their professional skills but also contributes to personal growth and job satisfaction. Nurses in this field often report a high level of satisfaction due to the meaningful connections they develop with their patients and the visible impact of their care.
Enhanced Patient Relationships
The holistic nursing model fosters stronger relationships between nurses and patients. By focusing on the person as a whole and spending time understanding their unique needs and life circumstances, nurses can build trust and rapport that facilitate better communication and cooperation from patients. This relationship-building is crucial for effective healthcare delivery, particularly in managing chronic conditions or in palliative care, where understanding and trust are paramount. Holistic nurses, by prioritizing these relationships, often see improved compliance with treatment plans and more positive health outcomes.
Challenges and Considerations Being a Holistic Nursing Specialist
Ethical and Legal Issues
Holistic nursing often faces ethical and legal challenges. Nurses must navigate the fine line between providing holistic care and adhering to medical regulations. Ensuring patient safety while using alternative therapies is crucial. Additionally, there are legal concerns about the scope of practice and the use of treatments that may not be widely accepted or scientifically proven.
Integration with Conventional Medicine
Combining holistic nursing with conventional medicine can be difficult. Some healthcare professionals are skeptical about the value of holistic approaches. This skepticism can create barriers to collaboration and integration. Holistic nurses must work hard to demonstrate the benefits of their methods and find common ground with traditional medical practices.
Overcoming Barriers to Practice
Holistic nursing consultations often take longer than standard medical appointments, which can be a challenge. Insurance may not cover the full cost of these extended sessions, making it hard for patients to afford holistic care. Furthermore, many holistic treatments lack sufficient research, making it tough to identify which methods are truly effective. Holistic nurses must stay informed and advocate for more research in their field.
Future Trends in Holistic Nursing
Technological Advancements
The future of holistic nursing will see more technology being used to help patients. New tools and gadgets will make it easier for nurses to care for people in a whole-person way. These advancements will help nurses keep track of patients’ health and make better care plans.
Research and Evidence-Based Practice
More studies will be done to show how well holistic nursing works. This research will help prove that holistic methods are good for patients. Nurses will use this information to improve their care and make sure they are using the best methods.
Global Perspectives and Expansion
Holistic nursing will grow in many parts of the world. Different countries will share their ideas and ways of caring for patients. This will help nurses learn from each other and provide better care everywhere.
Conclusion
Throughout this article, we have explored the intricate and rewarding world of holistic nursing, delving into its foundational principles, the roles and responsibilities of holistic nursing specialists, and the educational pathways that lead to this fulfilling career. By emphasizing the integration of physical, emotional, mental, and spiritual health, a holistic nursing specialist not only enriches the patient’s journey toward healing but also fosters a profound sense of satisfaction and personal growth among nurses. The commitment to treating the whole person, advocating for self-care, and championing environmental stewardship underscores the unique and pivotal role of holistic nursing specialists in transforming healthcare.
The exploration of holistic nursing’s core principles, educational requirements, and diverse work environments highlights its significance in modern healthcare—a beacon for those seeking to meld the science of medicine with the art of healing. As the healthcare landscape continues to evolve, the demand for such comprehensive care models is undeniable, paving the way for a future where holistic nursing is integral to patient care strategies. For aspiring holistic nurses, the journey is not just about acquiring the necessary certifications but embracing a philosophy that transcends traditional nursing practices, promising a career that is not only professionally rewarding but personally enriching. With every patient interaction and educational achievement, holistic nurses are at the forefront of a healthcare revolution, making a lasting impact on individuals and communities alike.
Becoming a Holistic Nursing Specialist is surprisingly easy, if you have the right mindset for it. Our Holistic and Integrative Health Care certification program requires a candidate to already have their Registered Nursing (RN) license. They then take 6 online Holistic Health Care Courses in order to meet the requirements to become a certified holistic nursing specialist. For full details about our online holistic nursing courses as well as our Certification program in Holistic Health Care, please visit our site here.
FAQs
- What is holistic nursing?
Holistic nursing is a type of nursing that focuses on treating the whole person. This means looking at a patient’s physical, mental, emotional, spiritual, and environmental health, rather than just their symptoms. - What does a holistic nurse do?
Holistic nursing is a healthcare profession where nurses provide comprehensive care, focusing on the whole person rather than just specific health issues. Holistic nurses assess patients’ lifestyles and overall well-being to guide their health and wellness strategies. - Is holistic nursing considered a specialized field?
Yes, holistic nursing is officially recognized as a specialty practice by the American Nurses Association since 2006, drawing on principles established by Florence Nightingale. - What are the qualifications required to become a certified holistic nurse?
To be eligible for certification in holistic nursing, one must have an unrestricted RN license, a degree from an accredited nursing program, and have completed at least 48 hours of education related to holistic nursing, including theory, research, and practice. - How do holistic nurses exemplify healthy living?
Holistic nurses promote health and healing by acknowledging and respecting each individual’s physical, mental, emotional, spiritual, and environmental strengths and challenges. They also honor each person’s health beliefs and experiences, serving as role models for healthy and holistic living. - Where do holistic nurses work?
Holistic nurses can work in many places including hospitals, private practices, wellness centers, and even patients’ homes. They can work with all types of patients, from children to the elderly. - Is holistic nursing recognized as a specialty?
Yes, holistic nursing is recognized as a specialty by the American Nurses Association. This means it has its own set of standards and guidelines that nurses must follow. - What are the benefits of becoming a holistic nursing specialist?
A Holistic Nursing Specialist can help lead to better patient outcomes and higher satisfaction. It also provides personal fulfillment for nurses and can positively impact the community by promoting overall wellness.
Research Articles:
Rationing of nursing care, a deviation from holistic nursing: A systematic review. Lata Mandal MSc Nursing, Et Al. Nursing Philosophy Volume21, Issue1 Special Issue: Missed care, care left undone: Organisation ethics and the appropriate use of the nursing resource January 2020 e12257
Access link here
Identifying Holistic Nursing Research Priorities for 2023–2026. Freysteinson WM, Enzman Hines M, Wind Wardell D, et al. Journal of Holistic Nursing. 2024;42(2):182-201.
Access link here
Spiritual Self-Care Management for Nursing Professionals: A Holistic Approach. Nilsson H. Et Al. Journal of Holistic Nursing. 2022;40(1):64-73.
Access link here
Utilization of Art in Nursing Education to Enhance Student Spiritual Growth and Holistic Nursing Practice. Kowalski SL, Et Al. Journal of Holistic Nursing. 2024;0(0).
Access link here