By – James M. Katz, BA
In our quest for holistic wellness advice, we’re always on the lookout for natural solutions that can make a real difference in our health. That’s where berberine comes in – a powerful compound found in several plants that’s causing quite a stir in the world of integrative medicine. We’ve seen its potential to have an impact on everything from metabolic health to heart health, making it a fascinating subject for those of us interested in holistic wellness tips and activities.
As we dive into the benefits of berberine, we’ll explore how it works to improve our overall well-being. We’ll look at its role in managing type 2 diabetes and insulin resistance, its potential to help with weight loss, and how it supports our cardiovascular system. We’ll also discuss berberine’s effects on digestion and gut health, and touch on how to take berberine for optimal results. By the end of this holistic guide to wellness, we hope you’ll have a clearer picture of how berberine might fit into your own health journey.
Understanding Berberine’s Holistic Wellness Approach
Definition of Holistic Wellness
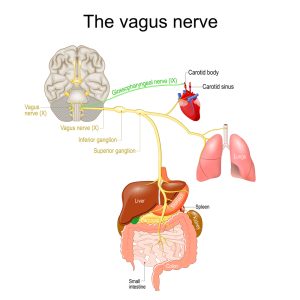
Holistic wellness is an approach that considers the whole person – body, mind, and spirit – in the quest for optimal health and well-being. It’s about looking at the big picture and addressing the root causes of health issues rather than just treating symptoms. In this context, berberine fits perfectly into the holistic wellness paradigm.
Berberine is a powerful compound found in several plants, including European barberry, goldenseal, and Oregon grape. It has been used for centuries in traditional Chinese and Ayurvedic medicine to treat various ailments. Today, it’s gaining recognition in integrative medicine for its potential to support overall health and wellness.
Berberine’s Multi-faceted Effects
What makes berberine particularly interesting from a holistic wellness perspective is its multi-faceted effects on the body. It doesn’t just target one specific area but has a wide-ranging impact on various aspects of health. One of the most significant ways berberine works is by activating an enzyme called AMP-activated protein kinase (AMPK). This enzyme is often referred to as the body’s “metabolic master switch” because it plays a crucial role in regulating energy balance and metabolism at the cellular level. When berberine activates AMPK, it sets off a cascade of metabolic processes that help the body use energy more efficiently.
This activation of AMPK has several downstream effects. It improves insulin sensitivity, making cells more responsive to insulin, which is key for maintaining healthy blood sugar levels. This is why berberine has shown promise in supporting metabolic health, particularly for those with type 2 diabetes or insulin resistance.
But berberine’s benefits don’t stop there. It also has a positive impact on heart health by helping to lower cholesterol levels and supporting healthy blood pressure. Some studies have shown that berberine can reduce total cholesterol, LDL (bad) cholesterol, and triglycerides while increasing HDL (good) cholesterol.
Moreover, berberine has been found to have anti-inflammatory and antioxidant properties, which can help protect against chronic diseases and support overall wellness. It also supports digestive health by promoting a healthy gut microbiome, which is increasingly recognized as crucial for overall well-being.
Why using Berberine is excellent Holistic Wellness Advice
Given its wide-ranging benefits, berberine can be a valuable addition to many holistic wellness routines. However, it’s important to remember that berberine is not a magic bullet. It works best when combined with other healthy lifestyle practices.
For those looking to incorporate berberine into their wellness routine, it’s typically taken as a supplement. The common dosage is 500 mg, taken two to three times a day before meals. However, it’s crucial to consult with a healthcare provider before starting any new supplement regimen, especially if you’re taking other medications, as berberine can interact with certain drugs.
Berberine for Metabolic Health
When it comes to holistic wellness advice, berberine stands out as a powerful ally for metabolic health. This natural compound has shown remarkable potential in supporting various aspects of metabolism, making it a valuable addition to integrative medicine approaches.
Blood Sugar Regulation
One of the most significant benefits of berberine is its ability to help regulate blood sugar levels. This is particularly important for those of us dealing with type 2 diabetes or at risk of developing it. Studies have shown that berberine can significantly lower blood sugar levels in people with type 2 diabetes. In fact, a 2008 study found that taking 1 gram of berberine per day lowered fasting blood sugar by 20%.
Berberine works through multiple mechanisms to help control blood sugar. It increases insulin sensitivity, promotes the breakdown of sugars inside cells, and even slows down the breakdown of carbohydrates in the gut. What’s really interesting is that berberine’s glucose-lowering effects are only apparent under hyperglycemic conditions. This means it’s less likely to cause hypoglycemia, which is a common concern with some diabetes medications.
Insulin Sensitivity
Improving insulin sensitivity is crucial for metabolic health, and berberine shines in this area too. It helps our cells respond better to insulin, which is key for maintaining healthy blood sugar levels. By increasing insulin sensitivity, berberine promotes better glucose uptake by our cells. What’s fascinating is that berberine has been found to be as effective as certain oral diabetes drugs in managing blood sugar levels. This doesn’t mean we should replace our prescribed medications, but it does highlight berberine’s potential as a complementary approach in our holistic wellness routine.
Lipid Profile Improvement
Beyond blood sugar control, berberine also has a positive impact on our lipid profile. This is crucial for heart health, which is often a concern for those of us dealing with metabolic issues. Studies have shown that berberine can help lower total cholesterol, LDL (bad) cholesterol, and triglycerides while increasing HDL (good) cholesterol.
In one study, taking 500 mg of berberine two to three times daily for three months led to a reduction in total cholesterol levels by up to 29%. This improvement in lipid profile can have a significant impact on our overall cardiovascular health. It’s important to note that while berberine shows promise in supporting metabolic health, it’s not a magic solution. As with any holistic wellness approach, it works best when combined with other healthy lifestyle practices like a balanced diet and regular exercise.
When considering berberine supplementation, it’s typically taken in doses of 500 mg, two to three times a day before meals. However, it’s crucial to consult with a healthcare provider before starting any new supplement regimen, especially if we’re taking other medications. In conclusion, berberine offers a holistic approach to metabolic health by supporting blood sugar regulation, improving insulin sensitivity, and enhancing lipid profiles. As we continue to explore integrative medicine and holistic wellness tips, berberine stands out as a promising natural compound that can complement our efforts to maintain optimal metabolic health.
Weight Management with Berberine
As we explore holistic wellness advice, berberine has gained attention for its potential role in weight management. While research is ongoing, some studies suggest that berberine might help with weight loss and body composition improvements.
Mechanisms for Weight Loss
Berberine’s potential for weight management stems from its effects on metabolism and energy balance. It activates an enzyme called AMP-activated protein kinase (AMPK), often referred to as the body’s “metabolic master switch.” This activation can lead to improved insulin sensitivity and more efficient energy use in cells.
A 2020 review of 35 studies from 2006-2019 indicated that berberine might be effective in reducing and preventing obesity. Another study from 2022 concluded that berberine could help with long-term weight loss and obesity prevention. These findings are promising, but it’s important to note that more high-quality research is needed to fully understand berberine’s effects on weight.
Interestingly, a 2023 study referred to a clinical trial where participants with obesity took 1.5 grams of berberine daily for 24 weeks. The results showed significant reductions in both BMI and waist circumference. However, we should interpret these results cautiously, as individual responses can vary.
Comparison to Conventional Methods
When comparing berberine to conventional weight loss methods, it’s crucial to maintain realistic expectations. While some have dubbed berberine “nature’s Ozempic,” this comparison may be overstated. Ozempic, a prescription medication for type 2 diabetes that can also lead to weight loss, works differently from berberine.
Ozempic slows down digestion, while berberine primarily influences how the body breaks down and uses energy. Unlike Ozempic, berberine is a dietary supplement that hasn’t undergone FDA approval for weight loss. This means there’s less robust evidence supporting its effectiveness for weight management compared to FDA-approved medications.
Dr. Wajahat Mehal, Co-director of the Yale New Haven Health Center for Weight Management, suggests that the impact of berberine on weight loss might be modest. He states, “If we take somebody who is moderately overweight, they’re probably looking at if anything, five to six pounds weight loss”. This underscores the importance of maintaining realistic expectations when considering berberine for weight management.
Lifestyle Integration
Integrating berberine into a holistic wellness routine requires careful consideration. It’s not a magic solution for weight loss and works best when combined with other healthy lifestyle practices. A balanced diet and regular exercise remain fundamental to any weight management plan. If you’re thinking about adding berberine to your wellness routine, it’s typically taken in doses of 500 mg, two to three times a day before meals. However, it’s crucial to consult with a healthcare provider before starting any new supplement regimen, especially if you’re taking other medications.
It’s worth noting that berberine may cause some side effects, primarily gastrointestinal symptoms such as nausea, abdominal pain, bloating, constipation, or diarrhea. These effects are generally mild and uncommon, but they’re important to be aware of. Remember, the goal of holistic wellness is to improve overall health, not just to lose weight. As Dr. Mehal points out, “I always say it’s of no importance to me what someone’s weight is, or what their waist circumference is or anything like that. But we know that both are tightly associated with diseases like diabetes, fatty liver, high blood pressure and stroke, which of course we care a lot about”.
In conclusion, while berberine shows promise for weight management, it’s just one piece of the holistic wellness puzzle. Integrating it into a comprehensive approach that includes a healthy diet, regular exercise, and other lifestyle factors is key to achieving and maintaining optimal health.
Cardiovascular Support
As we delve deeper into holistic wellness advice, it’s crucial to explore berberine’s potential benefits for heart health. Research suggests that berberine may offer significant support for cardiovascular health through various mechanisms.
Cholesterol Management
One of the most promising aspects of berberine is its ability to help manage cholesterol levels. Studies have shown that berberine can have a positive impact on lipid profiles, which is essential for maintaining heart health. In a meta-analysis of 16 clinical trials involving 2,147 patients with hyperlipidemia, researchers found that berberine significantly reduced levels of total cholesterol by 0.47 mmol/L, LDL cholesterol by 0.38 mmol/L, and triglycerides by 0.28 mmol/L.
Another systematic review of 11 clinical trials with 874 patients suffering from hyperlipidemia, type 2 diabetes, or both, revealed that berberine was associated with significant reductions in total cholesterol (0.61 mmol/L), triglycerides (0.50 mmol/L), and LDL cholesterol (0.65 mmol/L) compared to the control group. These findings suggest that berberine could be a valuable addition to holistic wellness strategies for managing cholesterol levels.
Blood Pressure Regulation
High blood pressure is a significant risk factor for heart disease, and berberine shows promise in this area as well. Some studies indicate that berberine may help lower both diastolic and systolic blood pressure. This effect could be particularly beneficial for those with type 2 diabetes, as hyperglycemia and hypertension often coexist and are considered leading risk factors for vascular disease in diabetic patients.
In one study, chronic administration of 100 mg/kg/day berberine not only lowered blood glucose but also reduced blood pressure and improved vasodilation in diabetic rats. While more research is needed to confirm these effects in humans, these findings suggest that berberine might offer a holistic approach to managing both blood sugar and blood pressure.
Arterial Health
Berberine’s cardiovascular benefits extend to arterial health as well. Research indicates that berberine may help improve vascular endothelial function, which is crucial for maintaining healthy arteries. In a recent animal experiment, berberine (50 mg/kg/d) was found to partly reduce blood pressure and circulating endothelial microparticles level in spontaneously hypertensive rats.
Moreover, berberine maintained arterial elasticity by reducing aortic pulse wave velocity and increasing the content of arterial media elastin fiber, indicating improved endothelium-dependent vasodilation. These effects suggest that berberine could play a role in protecting against arteriosclerosis and endothelial damage caused by hypertension.
It’s important to note that while these findings are promising, more research is needed to fully understand berberine’s effects on cardiovascular health in humans. As with any supplement, it’s crucial to consult with a healthcare provider before incorporating berberine into your holistic wellness routine, especially if you’re taking other medications or have existing health conditions.
In conclusion, berberine shows potential as a holistic wellness tool for supporting cardiovascular health. Its ability to help manage cholesterol levels, regulate blood pressure, and support arterial health makes it an intriguing option for those looking to take a comprehensive approach to heart health. However, it’s essential to remember that berberine should be part of a broader strategy that includes a balanced diet, regular exercise, and other lifestyle factors that promote overall well-being.
Digestive and Gut Health
As we explore holistic wellness advice, it’s crucial to understand the impact of berberine on digestive and gut health. This natural compound has shown promising effects in supporting a healthy digestive system and maintaining gut balance.
Antimicrobial Properties
One of the key benefits of berberine for digestive health lies in its antimicrobial properties. Research has shown that berberine can effectively combat various harmful bacteria, including methicillin-resistant Staphylococcus aureus (MRSA). In fact, studies have demonstrated that berberine can enhance the inhibitory efficacy of antibiotics against clinical multi-drug resistant isolates of MRSA. Berberine’s antimicrobial action seems to work by removing harmful bacteria in the gut, which in turn promotes the growth of beneficial bacteria. This dual action of eliminating harmful microbes while supporting beneficial ones makes berberine a valuable tool in maintaining a healthy gut environment.
Gut Microbiome Balance
The gut microbiome plays a crucial role in our overall health, influencing everything from digestion to immune function. Berberine has shown the potential to positively shape the composition and metabolism of the gut microbiota. This interaction between berberine and the gut microbiome is particularly interesting because it may explain some of berberine’s wide-ranging health benefits.
Studies have found that berberine can increase the proportion of beneficial bacteria in the gut. For instance, in a study involving db/db mice, berberine treatment increased the proportion of short-chain fatty acid (SCFA) producing bacteria such as Butyricimonas, Coprococcus, and Ruminococcus. These SCFAs are known to have numerous health benefits, including improved blood glucose control and enhanced insulin secretion.
Moreover, berberine has been shown to increase the relative levels of probiotic Lactobacillaceae, which has a negative correlation with the risk of type 2 diabetes. This suggests that berberine’s effects on gut microbiota could be part of its mechanism in supporting metabolic health.
Digestive Disorder Relief
Berberine shows promise in providing relief for various digestive disorders. Its ability to modulate the gut microbiome and its anti-inflammatory properties make it a potential holistic wellness tool for managing conditions like ulcerative colitis.
In animal studies, berberine has been shown to alleviate dysbiosis in rats with dextran sodium sulfate (DSS)-induced colitis. It significantly upregulates beneficial bacteria like Bacteroides and Akkermansia while decreasing the expression of conditionally pathogenic bacteria. This rebalancing of the gut microbiome could be beneficial in managing inflammatory bowel conditions.
Furthermore, berberine has shown potential in treating Helicobacter pylori infections, a common cause of ulcers. When added to standard treatment regimens, berberine might work as well as other accepted treatments for this condition. It’s important to note that while these findings are promising, more research is needed to fully understand berberine’s effects on digestive health in humans. As with any supplement, it’s crucial to consult with a healthcare provider before incorporating berberine into your holistic wellness routine, especially if you’re taking other medications or have existing health conditions.
In conclusion, berberine’s antimicrobial properties, its ability to balance the gut microbiome, and its potential to provide relief from digestive disorders make it an intriguing option for those looking to support their digestive and gut health. As we continue to explore integrative medicine and holistic wellness tips, berberine stands out as a promising natural compound that can complement our efforts to maintain optimal digestive health and overall well-being.
Conclusion
Berberine has shown its potential as a versatile tool to enhance overall wellness. Its ability to regulate blood sugar, improve cardiovascular health, and support digestive function makes it a promising addition to holistic health routines. What’s more, berberine’s impact on weight management and metabolic health highlights its role in addressing some of the most common health concerns today.
As we continue to explore natural ways to boost our health, berberine stands out as a compound worth considering. However, it’s crucial to remember that berberine is just one piece of the puzzle. To truly embrace holistic wellness, we need to combine supplements like berberine with a balanced diet, regular exercise, and other healthy lifestyle choices. Always consult with a healthcare provider before adding new supplements to your routine, especially if you’re taking other medications.
The American Institute of Health Care Professionals offers a Certification Program in Holistic Healthcare open to students in the nursing profession. It is an excellent way to learn about the holistic wellness advice and other issues we have discussed here today. If you’re interested in becoming certified in holistic nursing then please review our Online Holistic and Integrative Healthcare Program.
FAQs
1. What effects does berberine have on the body?
Berberine plays a significant role in reducing inflammation through various mechanisms. It diminishes oxidative stress, curtails the production of inflammatory proteins, and aids in immune regulation. These anti-inflammatory properties suggest that berberine might be effective in treating conditions such as arthritis.
2. Why is berberine not commonly prescribed by doctors?
Berberine has the potential to interfere with prescription medications by altering their levels in the bloodstream, primarily because it affects certain liver enzymes involved in drug metabolism, like those that process metformin. Additionally, there’s a heightened risk of bleeding when using berberine.
3. Is long-term use of berberine safe?
Long-term consumption of berberine can be problematic due to its toxicity, which is higher in its pure form compared to plant extracts. Extended use can lead to liver function changes, stomach issues, toxicity to the liver and blood, inflammatory bleeding issues, immune cell damage, and triggered cell death.
4. How quickly can one expect to see benefits from taking berberine?
The benefits of berberine are typically observed over a period of about 90 days according to research studies. However, some individuals may notice improvements in their blood sugar levels as early as the first month of supplementation, whereas drugs like metformin tend to act more quickly.
Research Articles:
Anticancer Effects and Mechanisms of Berberine from Medicinal Herbs: An Update Review. Xiong R-G, et al. Molecules. 2022; 27(14):4523.
Access link here
Berberine: An Important Emphasis on Its Anticancer Effects through Modulation of Various Cell Signaling Pathways. Almatroodi, S.A.; Alsahli, M.A.; Rahmani, A.H. Molecules 2022, 27, 5889.
Access link here
Effects of Berberine on Atherosclerosis. Rui Rui, Yang Haolan, Et Al. Front. Pharmacol., 25 November 2021 Sec. Cardiovascular and Smooth Muscle Pharmacology
Access link here
Gut microbiome-related effects of berberine and probiotics on type 2 diabetes (the PREMOTE study). Zhang, Y., Gu, Y., Ren, H. et al. Nat Commun 11, 5015 (2020).
Access link here