I. Introduction
Substance abuse disorders pose a significant challenge to individuals and society at large, leading to detrimental impacts on physical health, mental well-being, and social relationships. The complexities of addiction necessitate a multifaceted approach to treatment that encompasses not only the cessation of substance use but also the comprehensive rehabilitation of the individual. Recent advancements in understanding the neurobiological underpinnings of addiction have paved the way for innovative treatment methodologies, including cognitive-behavioral therapy, medication-assisted treatment, and holistic healing practices. These evidence-based approaches have demonstrated effectiveness in promoting recovery and reducing the rates of relapse, yet they require careful customization to address the unique needs of each patient . As the landscape of addiction treatment continues to evolve, it is essential to explore proven strategies that facilitate lasting recovery, ultimately enabling individuals to break free from the chains of substance abuse and regain their lives (Nady el-Guebaly et al., 2020-11-03).
A. Definition of substance abuse disorders
Substance abuse disorders are mental health conditions characterized by an individual’s compulsive use of drugs or alcohol despite facing significant adverse consequences. These disorders encompass a spectrum of behaviors, including physical dependency and psychological addiction, which disrupt personal, social, and occupational functioning. The definition extends to various substances, both legal and illegal, highlighting the complexities of addiction and its biopsychosocial implications. Furthermore, the interplay between substance abuse and other disorders, such as gambling addiction, underscores the importance of comprehensive assessment and treatment strategies. For instance, individuals with substance use disorders often minimize their usage or conceal other addictions, complicating their assessment and care (P Čargonja et al., 2023). In particular, the treatment of pregnant women with opioid use disorder necessitates careful medication management to balance benefits and risks for both the mother and neonate (Singh S, 2025). Recognizing these intricacies is crucial for effective intervention and support in the recovery process.
B. Importance of addressing substance abuse
Addressing substance abuse is paramount not only for individual health but also for the broader societal fabric. The multifaceted nature of substance use disorders (SUDs) intertwines psychological, social, and economic factors, necessitating comprehensive intervention strategies that encompass prevention, treatment, and policy reform. Effective treatment approaches must consider the unique variables influencing each individuals experience with addiction, reflecting the complex etiopathogenesis identified in current research. Moreover, the socio-economic costs of neglecting substance abuse are significant, affecting community resources and overall public health. As noted in the literature, the absence of established guidelines for SUD management indicates a critical need for developed policies focused on both prevention and effective therapeutic measures, particularly for vulnerable populations (Victor A Voicu et al., 2025). By implementing collaborative care approaches and evidence-based treatment, society can not only alleviate the burden of SUDs but also foster healthier communities, highlighting the urgency of addressing this pervasive issue (Stanford M et al., 2014).
C. Overview of treatment approaches
Treatment approaches for substance use disorders (SUDs) are inherently multifaceted, necessitating the integration of various methodologies to effectively address the complexity of addiction. These approaches typically encompass a combination of pharmacological interventions, behavioral therapies, and holistic practices aimed at fostering long-term recovery. For instance, medication-assisted treatment (MAT) has shown promise in reducing cravings and withdrawal symptoms, while cognitive-behavioral therapy (CBT) equips individuals with essential skills to manage triggers and develop coping strategies. Moreover, the importance of community support and engagement cannot be overstated; collaborative frameworks that involve multiple stakeholders can enhance the efficacy of treatment protocols. As noted in recent literature, the need for coherent guidelines and policies regarding SUD treatment is urgent, particularly for vulnerable populations, underscoring the demand for evidence-based practices in healthcare settings (Victor A Voicu et al., 2025) (Stanford M et al., 2014). Consequently, a comprehensive understanding of these approaches is vital for effective intervention strategies.
II. Understanding Substance Abuse Disorders
The complexity of substance abuse disorders necessitates a multifaceted understanding of their underlying causes and effects. These disorders are not merely issues of individual choice; they represent chronic diseases influenced by genetic, environmental, and social factors, complicating both prevention and treatment efforts (Ali MO, 2023). As the prevalence of substance use disorders continues to rise, particularly among diverse populations, the need for culturally competent interventions becomes increasingly critical. Multicultural counseling skills are essential for practitioners, as the nation’s demographic landscape evolves, with projected statistics indicating significant growth in minority populations by 2050 (Boyd L et al.). Addressing substance abuse disorders through a multicultural lens can enhance the effectiveness of treatment programs and foster recovery in clients. Thus, understanding the intricate relationships between substances, individuals, and their environments is pivotal for developing robust strategies aimed at breaking free from the cycle of addiction.
A. Causes and risk factors
Understanding the causes and risk factors associated with substance abuse disorders is crucial in developing effective treatment modalities. Various interrelated factors contribute to an individuals vulnerability, including genetic predispositions, environmental influences, and early exposure to drugs. For instance, research shows that individuals with a family history of substance abuse are more likely to develop similar disorders, underscoring the role of genetics in addiction ((Ali MO, 2023)). Additionally, environmental elements such as peer pressure, trauma, and socioeconomic status can exacerbate the risk of addiction, particularly among adolescents. Anxiety disorders, including Generalized Anxiety Disorder (GAD), further complicate this landscape, as they can lead to increased substance use as a form of self-medication ((Roy A et al., 2025)). Recognizing these multifactorial causes not only aids in the comprehension of substance use disorders but is essential for creating targeted interventions that address both psychological and situational factors.
B. Psychological and physical effects
The psychological and physical effects of substance abuse can be profound and multifaceted, often deteriorating both mental health and bodily well-being. Individuals who have experienced early life adversity (ELA) are particularly susceptible, as research indicates that such backgrounds significantly heighten vulnerability to both the pleasurable and adverse effects of psychoactive substances. Those with higher ELA scores tend to report more intense positive experiences but also face severe negative repercussions, including emotional disturbances and physical health issues (M Carlyle et al., 2025). Moreover, the specific case of zolpidem dependence reveals similarly detrimental outcomes, wherein individuals exhibited significant memory impairment and social deficits tied to escalating dosages (Leal G et al., 2024). These intertwined psychological and physical effects underscore the complexity of treating substance abuse disorders, emphasizing the necessity for personalized treatment approaches that address both the enticing highs and the debilitating lows associated with addiction.
C. The impact on families and communities
The impact of substance abuse disorders resonates deeply within families and communities, significantly altering their dynamics and overall health. Families often bear the brunt of emotional and financial strain, as relatives of individuals struggling with addiction may experience heightened stress levels and increased instances of domestic conflict. Furthermore, exposure to adverse childhood experiences (ACEs) due to parental substance abuse can perpetuate a cycle of trauma that affects subsequent generations, leading to various psychiatric disorders, including depression and substance abuse itself (T Mu Bñoz et al., 2025). Communities, in turn, face challenges such as increased crime rates, healthcare costs, and stigma surrounding addiction, which can hinder individuals from seeking help. However, initiatives funded by opioid crisis grants, such as those in Ohio, have demonstrated the potential for community-driven change. These endeavors have not only increased awareness and treatment accessibility but have also improved the collective understanding of substance use disorders, fostering a supportive environment for recovery (R T Sherba et al., 2023).
III. Evidence-Based Treatment Approaches
The integration of evidence-based treatment approaches is crucial for effectively addressing substance abuse disorders, as these strategies are grounded in rigorous research and clinical outcomes. One of the most significant findings relates to the role of genetic factors, particularly the dopamine transporter gene polymorphism (SLC6A3), which has shown a notable association with personality disorders that often co-occur with substance abuse disorders (Vogiatzoglou A et al., 2024). Furthermore, Cognitive Behavioral Therapy (CBT) stands out as a leading methodological framework in psychotherapy, extensively proven to be effective in managing psychological health conditions, including substance misuse disorders. By focusing on the interplay of thoughts, feelings, and behaviors, CBT provides a structured approach that empowers individuals to challenge and change detrimental patterns while promoting sustainable recovery (Irmak Çavuşoğlu, 2024). Together, these evidence-based approaches emphasize the importance of personalized treatment plans tailored to each patients unique profile, fostering a more significant potential for long-term healing and resilience.
A. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) has emerged as a pivotal approach in treating substance abuse disorders, demonstrating significant efficacy in enhancing abstinence self-efficacy among individuals grappling with addiction. Research indicates that CBT, when tailored to the specific needs of patients, can effectively facilitate behavioral changes that promote recovery. In a study comparing CBT based on Marlatts Model with other therapeutic interventions, findings revealed that participants in the CBT group experienced a marked increase in abstinence self-efficacy scores, advancing from a baseline of 44.60 to 61.85, underscoring its practicality in long-term addiction management (Davoudabadi Z et al., 2024). Furthermore, the psychological underpinnings of CBT address co-occurring issues, such as depression and body image concerns, which can exacerbate substance use disorders. By integrating CBT into treatment regimens, individuals can gain essential coping strategies, bridging the gap between mental health and recovery, ultimately leading to a more holistic approach to addiction treatment (Rad MK et al., 2024).
B. Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) is a major advance for managing substance abuse disorders. It specifically helps people with opioid dependence. MAT mixes medicine with counseling and behavioral therapies. This creates a full treatment plan. It addresses the physical and mental sides of addiction. Research shows MAT improves recovery results. It reduces withdrawal symptoms and cravings, so patients stay sober. Substance use rates are high in regions like Nigeria and South Africa. Adding MAT to current treatment programs is important there. Statistics from the UNODC World Drug Report 2023 are alarming. They show an urgent need for effective treatments in these areas. We must also consider other mental health conditions. Body Dysmorphic Disorder has complex links with substance abuse. We need gender-specific and trauma-informed care plans (Olowoyo-Richards AT, 2025), (Metin Çınaroğlu, 2024).
C. Motivational Interviewing (MI)
Motivational Interviewing (MI) is a key technique for treating substance abuse disorders. It uses a client-centered approach to build internal motivation for change. This method encourages individuals to examine their mixed feelings about substance use. They gain a clear understanding of their personal goals and values. Research shows that MI strengthens commitment to change. It also works well with other therapies like cognitive behavioral therapy (CBT). Clients see improved results. Interventions for substance use among intimate partner violence (IPV) perpetrators report positive outcomes with MI. This shows its value in various contexts (Sousa M et al., 2024). MI also works for Internet use disorders (IUDs). This proves it applies to many forms of addiction (Pape M et al., 2023). MI is a central part of evidence-based strategies for ending the cycle of substance abuse.
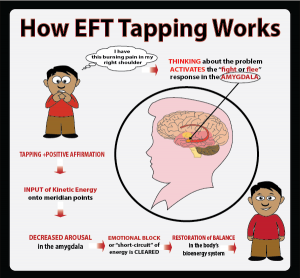
IV. Holistic and Alternative Therapies
Holistic and alternative therapies gain attention as complementary treatments for substance abuse disorders. They look beyond simple symptom management to understand addiction fully. These methods highlight the link between mind, body, and spirit. They create a personal treatment setting that meets the specific needs of each patient. For example, programs often include meditation, yoga, and nutritional counseling. These methods improve recovery results by building self-awareness and resilience. Practitioners use this combined method to address the biological, psychological, social, and spiritual sides of addiction. This allows for a more detailed treatment plan. This strategy supports research on the value of addressing diverse needs with a complete model. It improves options for people with substance abuse disorders (MD JU-S et al., 2025), (Jorgensen D, 2015).
A. Mindfulness and meditation practices
Mindfulness and meditation are key parts of treating substance abuse disorders. This occurs mainly through Mindfulness-Based Relapse Prevention (MBRP). This method mixes standard cognitive-behavioral techniques with mindfulness meditation. It helps people build awareness and coping strategies during recovery. Research shows that mindfulness meditation improves the ability to handle negative emotions. It reduces stress and lowers cravings. These are big challenges for people recovering from addiction (Bowen S et al., 2011). MBRP builds a compassionate relationship with thoughts and feelings. This lets people respond to triggers differently. It lowers the chance of relapse (Witkiewitz K et al., 2005). These practices are becoming more common. Their use in therapy shows promising results. This highlights their value as a full tool for stopping substance dependence. More study of these methods could explain their success. It could show practical uses for treating addiction.
B. Art and music therapy
Art and music therapy are powerful tools against substance abuse disorders. They offer new ways to express and heal. These methods let individuals explore complex emotions linked to addiction. This aids personal insight and emotional control. Art therapy encourages participants to visualize and externalize feelings. This leads to deep personal changes and self-awareness. Music therapy improves social, cognitive, and behavioral functions. It helps individuals manage anxiety and trauma from substance use (N/A). Structured music activities improve communication and social skills. They build connections needed for recovery (McChesney A et al., 2013). People engage with these outlets and develop healthier coping habits. This supports their path toward sobriety and growth.
C. Exercise and nutrition as recovery tools
Adding exercise and nutrition to recovery programs changes the treatment of substance abuse disorders. Physical activity improves mood and reduces stress. These are critical factors in recovery. Regular exercise releases endorphins. This promotes feelings of well-being. It helps fix the emotional instability often linked to addiction. Nutrition matters for recovery too. A balanced diet supports physical health and brain function. This creates a strong base for sobriety. Strategies like lifestyle medicine show the value of changeable habits like diet and activity. These factors are necessary. They prevent and treat substance abuse and mental health issues (Farrokhi M et al., 2024). Using these elements fits with treatments that consider the entire person. They address the connection between mind and body. Non-drug methods for alcohol use disorder prove this (Valida B et al., 2023).
V. Conclusion
Treating substance abuse disorders requires many different approaches. A complete plan is necessary for effective intervention and recovery. We must prioritize research and development as recent studies suggest. This leads to specific treatment programs for groups like children and adolescents. These programs also focus on long-term management in the community (Kim H et al., 2024). Policy changes have worked well. Medicaid IMD exclusion waivers improved access to integrated care. This helps patients with both mental health and substance use issues. Results differ based on who owns the facility. This proves the need for specific methods to make treatment available to all (Ge Y et al., 2024). Everyone involved must work together. Ongoing research and policy reform are required to fight substance abuse disorders.
A. Summary of effective treatment strategies
Treatment strategies for substance abuse disorders need a complete approach. This method must address the many different sides of addiction. These strategies rely on accepting the link between cultural beliefs and treatment success. This is true in African settings. There, wrong ideas about witchcraft can block recovery efforts. (Matheba CM, 2025) shows that these deep beliefs require teamwork. Professional social workers, traditional healers, and religious leaders must work together. They can create culturally aware plans. We must also address dual diagnosis. This happens when mental health disorders occur alongside substance abuse. Treating both promotes good results, especially among young people. The data in (Udemezue K katas et al., 2024) show that combined treatment models work best. These mix psychiatric care with behavioral therapies. They prove more effective than separate approaches. We must understand and address these many factors. This step helps build effective treatment plans. Then, people battling substance abuse disorders can reach lasting recovery.
B. The importance of personalized treatment plans
Personalized treatment plans are vital for substance abuse treatment. Providers design these plans to meet the unique needs of each individual. They recognize that substance use disorders appear differently in different groups. These approaches review personal histories, co-occurring mental health conditions, and socio-economic factors. This method increases engagement and improves treatment results. Research shows that tailored interventions make long-term recovery more likely. They address the root causes of substance use rather than focusing just on the addictive behavior. Clients also provide feedback during the treatment process. This creates a shared environment. It helps people take charge of their recovery and strengthens their commitment (Sassaman W, 2025-03-21). Personalized treatment plans are a major step in treating substance abuse disorders. They emphasize a complete view of the healing process.
C. Future directions in substance abuse treatment research
Substance abuse treatment changes constantly. Future research will explore new, combined approaches to improve recovery results. Experts will likely focus on personalized treatment plans that consider genetic, psychological, and social factors. This shift recognizes how these elements mix in individual addiction experiences. New technology will also help. Telehealth, mobile apps, and artificial intelligence can make care easier to find. These tools reduce barriers like location and stigma. Scientists will also study brain treatments. Specific drugs and brain stimulation might help current therapies work better (Press A, 2013-05-20). Future studies should look at the full picture. This includes mind-body connections and community support. Research can then find lasting treatments for substance abuse disorders.
Additional AIHCP Blog “How to become a Substance Abuse Counselor” Click here
Additional Resources
Tyler, M. (2018). “An Overview of Addiction”. Healthline. Access here
Felman, A. “What are the treatments for addiction?”. Medical News Today. Access here
“Treatment of Substance Use Disorders”. (2024). CDC. Access here
“Addiction and the Brain”. Psychology Today. Access here














 Written by
Written by