I. Introduction
In recent years, the concept of holistic nursing has emerged as a pivotal approach within the healthcare landscape, emphasizing the interconnectedness of body, mind, and spirit in patient care. Holistic nursing transcends traditional medical practices by recognizing patients as complete beings rather than mere recipients of treatments. This comprehensive perspective fosters an environment where emotional and spiritual needs are acknowledged alongside physical ailments, thereby enhancing overall well-being. By integrating holistic principles, nurses can cultivate deeper relationships with their patients, leading to more effective and empathetic care. The practice is not merely a set of techniques; rather, it embodies a philosophy that encompasses compassionate presence, active listening, and individualized care strategies tailored to the unique circumstances of each patient . As such, understanding the essence of holistic nursing is essential for healthcare professionals aiming to provide impactful, person-centered care (2009).
Please also review AIHCP’s program in Holistic Nursing to become a certified Holistic Nurse
A. Definition of holistic nursing
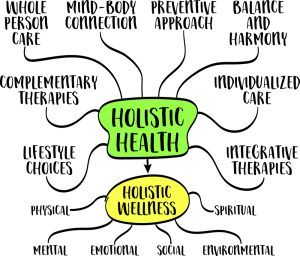
Holistic nursing represents an approach to health care that emphasizes the interconnectedness of mind, body, and spirit in the healing process. This philosophy extends beyond traditional medical practices, recognizing that a patient’s emotional, social, and spiritual needs are equally vital to their overall well-being. Holistic nurses advocate for patient-centered care that respects individual values and preferences while promoting health in a comprehensive manner. By integrating various therapeutic modalities, such as art therapy and guided imagery, holistic nursing seeks to empower patients in their journey towards health and wellness. This comprehensive framework not only addresses physical symptoms but also considers lifestyle factors, personal beliefs, and cultural contexts that influence an individual’s health experience. As such, holistic nursing challenges conventional paradigms by urging practitioners to foster deeper connections with their patients, ultimately enriching the practice of care itself (Smith MJ et al., 2015-02-20).
B. Importance of holistic approaches in healthcare
In recent years, holistic approaches have gained prominence in healthcare, emphasizing the interconnectedness of the mind, body, and spirit in promoting overall well-being. This comprehensive perspective is crucial, as it recognizes that patients are not merely recipients of care but individuals with unique experiences, emotions, and social contexts that influence their health outcomes. By addressing psychological, emotional, and spiritual needs alongside physical ailments, holistic nursing fosters a more personalized and compassionate care model. Furthermore, such an approach can enhance patient satisfaction, engagement, and adherence to treatment plans, thereby improving recovery rates and fostering long-term health. Studies have shown that holistic practices, including mindfulness, nutrition, and alternative therapies, significantly contribute to the efficacy of traditional medical treatments . This integration of holistic principles into healthcare practice not only facilitates disease management but also nurtures a culture of empathy and respect in the patient-provider relationship (Ross L et al., 2025-05-23).
C. Overview of the essay structure
In establishing a comprehensive exploration of holistic nursing within The Soul of Care: What is Holistic Nursing?, a clear and structured essay format is indispensable. The introductory section will lay the groundwork by defining holistic nursing and articulating its significance in contemporary healthcare. Following this, the body will be divided into subsections that delve into the key principles of holistic care, the role of triad leadership in promoting collaborative practices, and the integration of teaching methodologies for healthcare professionals. For instance, (Hill J et al., 2025) highlights how triad leadership cultivates an environment conducive to patient-centered care, thereby enhancing holistic approaches in nursing. Additionally, the examination of educational frameworks aimed at improving teaching skills among medical professionals underscores the necessity of effective communication in holistic practices, as suggested by (Darwin A et al., 2025). Ultimately, the conclusion will synthesize the insights gathered, reaffirming the value of holistic nursing in delivering compassionate care.
II. Historical Context of Holistic Nursing
The historical context of holistic nursing reflects a confluence of ancient practices and modern-day healthcare philosophies, emphasizing the significance of treating the patient as a whole rather than merely addressing symptoms. Historically, various cultures, including Indigenous communities, embraced holistic approaches that acknowledged the interconnectedness of mind, body, and spirit in health and healing . The formalization of holistic nursing as a practice began in the late 20th century, spurred by a growing recognition of the limitations of conventional biomedical models in promoting comprehensive patient care. Prominent figures such as Florence Nightingale laid the groundwork by advocating for a healing environment and the importance of the caregiver-patient relationship (Jones & Publishers B). This evolution has led to the integration of holistic principles into nursing curricula and practice, reinforcing the idea that empathetic, patient-centered care is foundational to effective nursing. Such advancements reflect an enduring commitment to nurturing the inherent dignity of each individual.
A. Origins of holistic nursing practices
The origins of holistic nursing practices can be traced back to ancient healing traditions that recognized the interconnectedness of body, mind, and spirit. Early practitioners, such as those in traditional Chinese medicine and Ayurveda, emphasized the importance of treating the whole person rather than merely addressing symptoms. These philosophies laid the groundwork for holistic approaches by fostering an understanding that emotional and spiritual well-being significantly influence physical health. In the 20th century, the emergence of holistic nursing as a formal discipline occurred alongside the evolution of patient-centered care models. Pioneering figures, such as Florence Nightingale, advocated for a more integrative approach to nursing that considered patients environmental, physical, and emotional contexts. This historical foundation has increasingly gained recognition, reflecting a shift in healthcare paradigms towards a more comprehensive and compassionate understanding of patient care (Alligood MR, 2021-07-23).
B. Evolution of nursing philosophies
The evolution of nursing philosophies has significantly shaped the practice of holistic nursing, emphasizing the importance of understanding a patients lived experiences beyond mere diagnostic labels. This shift reflects a philosophical commitment to interpretive phenomenology, which seeks to explore the essence of patient care through authentic engagement with their narratives. By recognizing how societal stigmas can limit empathetic care, nurses are encouraged to approach patients with a framework that prioritizes holistic well-being. Moreover, as the profession grapples with the demands of Diversity, Equity, and Inclusion, the introduction of the C.A.R.E. Framework underscores the need for a values-driven approach rooted in advocacy and social justice. By melding these evolving philosophies, nursing practice can transition towards a more comprehensive model, ultimately enhancing patient outcomes and reaffirming the professions dedication to caring as an ethical and human-centered practice (Doucette N et al., 2025), (Campbell S et al., 2025).
C. Key figures and movements in holistic nursing
Holistic nursing, an evolving field, has been significantly shaped by key figures and movements that promote a comprehensive framework for patient care. Pioneers such as Florence Nightingale laid the groundwork for holistic principles by emphasizing the importance of the environment and emotional well-being in nursing practice. Further advancements were made in the 1970s and 1980s when the holistic nursing movement began to gain momentum, largely due to the work of nurses like Dr. Jean Watson, who formulated the Theory of Human Caring, highlighting the interconnectedness of mind, body, and spirit in health. The emergence of organizations such as the American Holistic Nurses Association has formalized and expanded the practice, advocating for educational standards and ethical guidelines that address the multifaceted nature of health and wellness (Margaret A Burkhardt et al., 2024-06-07). Through these contributions, holistic nursing has matured into a discipline dedicated to fostering healing relationships that honor the whole person.
III. Principles of Holistic Nursing
At the core of holistic nursing lies a set of principles that prioritize the interconnectedness of the body, mind, and spirit in the healing process. Holistic nurses embrace a person-centered approach, recognizing that each patient is a unique individual with diverse experiences, beliefs, and needs that must be addressed in the care plan. This perspective emphasizes the importance of creating a therapeutic relationship, fostering open communication, and practicing empathy to support patients emotional and psychological well-being alongside their physical health. Moreover, holistic nursing incorporates complimentary therapies, such as mindfulness, nutrition, and physical activity, to promote overall wellness and balance within the individual. By understanding the intricate relationships between various aspects of health, holistic nurses strive to empower patients, guiding them toward self-care and resilience while acknowledging the complexities and nuances of their healing journeys (Ruth F Craven et al., 2019-12-26). This comprehensive approach underscores the essence of holistic nursing as the soul of care.
A. The mind-body-spirit connection
Holistic nursing fundamentally recognizes the profound relationship between the mind, body, and spirit, emphasizing that these components must be in harmony for optimal health and wellness. This integrated approach draws from ancient philosophical teachings, notably within Indian traditions, where practices such as meditation and yoga are instrumental in fostering this connection. Through these practices, individuals often discover that true wellness emanates from a balance among their mental, physical, and spiritual states (Thakur DK, 2025). Furthermore, contemporary research supports the notion that addressing these interconnected facets is crucial for mental health, as holistic interventions have demonstrated statistically significant improvements in patient outcomes compared to traditional methods (Kaushik D et al., 2024). Thus, the mind-body-spirit connection serves not only as a foundational principle of holistic nursing but also as a transformative framework that challenges reductionist views of health care, promoting a more comprehensive understanding of well-being and patient care.
B. Patient-centered care and individualized treatment
Patient-centered care (PCC) and individualized treatment are central to holistic nursing. This model addresses the diverse needs of patients and prioritizes their unique preferences and values. The interaction builds deeper engagement between healthcare providers and patients. It creates a space where individuals can openly discuss their health concerns and goals. Research in interventional oncology shows the effectiveness of PCC. It improves patient satisfaction and emotional well-being through custom treatment strategies, clear communication, and shared decisions (Devora L Stone et al., 2025). A sexuality education program for older adults showed major gains in sexual knowledge and self-efficacy. This result proves the value of addressing specific age-related concerns (B S Diggle-Fox et al., 2026). Holistic nursing uses these principles to build a responsive healthcare system. It honors the whole person and supports overall well-being.
C. The role of environment in healing
The environment profoundly influences the healing process. This setting is central to holistic nursing practices. A caring environment supports emotional and physical well-being. It helps patients feel safe and protected during their recovery. Elements like natural light, plants, and calm colors create a serene atmosphere. This atmosphere reduces stress and anxiety levels. The result is better health for patients. Sound is another factor. It serves as a tool for healing or a source of irritation. This fact requires mindful attention to the acoustic environment in healthcare settings (Douglas A Wengell et al., 2008). Holistic nursing designs spaces for comfort and peace. This approach meets immediate medical needs. It also supports emotional and spiritual health. A healing environment helps individuals begin their recovery. This practice represents the core principles of holistic care.
IV. Holistic Nursing Practices
Holistic nursing practices use a complete method for patient care. This moves beyond standard models and looks at physical, emotional, social, and spiritual health. This view helps providers connect deeply with patients. They see that illness affects the mind and spirit, not just the body. Holistic nurses use active listening, empathy, and kindness. They adjust care to fit the specific needs and wants of each patient (Dossey BM et al., 2015-05-23). These practices often include extra therapies like mindfulness, nutrition, and physical activity. These habits support well-being. The main goal is treating the whole person instead of just symptoms. This improves care quality. It helps patients heal and learn about themselves.
A. Integrative therapies and their applications
Holistic nursing pays new attention to integrative therapies. These methods come from ancient healing practices. They focus on the connection between mind, body, and spirit. Daivavyapashraya Chikitsa is a key example of this approach. This Ayurvedic model uses spiritual therapies like mantra chanting and sacred rituals. These practices support mental health and emotional strength. This model treats common mental health problems. It offers a path that works with standard medical treatments (Dr. Pareek A et al., 2025). Digital health technologies also offer new opportunities for holistic nursing. Mobile apps and telehealth services make care more personal and accessible. These new tools help build deeper relationships between patients and nurses. They keep the main goals of integrative care strong even with advanced technology (Swain M et al., 2025). Holistic nursing grows by mixing traditional wisdom with modern tools. This mix meets many patient needs. It also confirms that compassionate care remains the priority.
B. Communication techniques in holistic nursing
Holistic nursing requires effective communication techniques to build a compassionate and empathetic environment. These methods involve more than verbal exchanges. They include active listening, nonverbal cues, and attention to patient emotions. Nurses use tools like the NURSE model to improve empathy. This builds rapport and trust with patients and their families. Experiential learning strategies also strengthen these skills in nursing education. Simulation-based scenarios show that emotional intelligence is central to holistic care (Reis TH da Silva, 2025). Collaboration is required as well. Nurses coordinate care across disciplines to meet the many needs of patients. This integration helps patients have a full dialogue about their health. Such conversations assist with chronic pain management and well-being (Alsamti AI¹ et al., 2025). These communication techniques define holistic nursing and support patient-centered care.
C. The importance of self-care for nurses
Nursing is a demanding field. Self-care is crucial because it directly affects the quality of care patients receive. Holistic nursing recognizes that nurses must care for their own physical, emotional, and spiritual health first. They do this to support their patients well. Self-care lowers the risk of burnout. It also helps the nurse give compassionate and empathetic care. Research shows that nurses like their jobs more when they look after their own well-being. Patient outcomes improve too. This proves a link between nurse health and patient care. Spiritual care helps build emotional resilience in holistic nursing. It reduces depressive symptoms among caregivers. Putting self-care first fits with Orem’s Self-Care Deficit Theory and Roy’s Adaptation Model. These ideas show the strong connection between personal health and professional success (Yeh C-T et al., 2025), (Muhammad T, 2024).
V. Conclusion
Holistic nursing uses a complete approach to healthcare that connects the mind, body, and spirit. This method builds a deeper sense of compassion in caregivers and improves patient well-being. Recent studies show that nursing students, such as those in Indonesia, report good self-care habits. They succeed in emotional and spiritual areas, but they also note a need for better physical self-care techniques (Damayanti MR et al., 2025). Including creative arts in nursing education also helps students understand holistic care. This training encourages spiritual discovery and moral values like mercy and compassion (N/A, 2025). Focusing on these different parts of holistic nursing prepares future nurses to give empathetic care. It also helps them care for themselves, which creates a continuous cycle of wellness in healthcare settings. Building a holistic nursing system is necessary to improve both the practice of nursing and patient results.
A. Summary of key points
We finish our review of holistic nursing. Several key points show its nature and value in modern healthcare. This care connects the mind, body, and spirit. It treats patients as whole individuals, and it does not just fix physical problems. This view helps build meaningful relationships between nurses and patients. These bonds improve trust and treatment results. The practice also asks for personal care plans. These plans account for unique experiences, culture, and beliefs. Such factors affect health results (Peate I et al., 2022-07-18). The field also promotes self-care for practitioners. Nurses must watch their own well-being to support others. These steps improve patient satisfaction. They help create a compassionate and empathetic healthcare setting. This confirms that every part of a patient’s life affects their health and healing.
B. The future of holistic nursing in healthcare
The healthcare field changes constantly. The future of holistic nursing will integrate comprehensive care models. These models address the many needs of patients. Holistic nursing emphasizes the physical aspect of health. It also includes emotional, spiritual, and social dimensions. This focus reflects a move toward patient-centered practices. Providers prioritize well-being over simple symptom management. Recognition of the limits of traditional biomedical methods drives this change. This is true for chronic disease management. A deep understanding of the patient’s experience is crucial there. Technology also helps. Telehealth and digital health tools allow nurses to provide holistic care remotely. These tools support ongoing connections with patients (Eliopoulos C, 2013-05-24). Holistic nursing gains prominence. It may lead to improved health outcomes and greater patient satisfaction. The practice redefines the nature of care in modern settings.
C. Final thoughts on the impact of holistic nursing on patient care
Adding holistic nursing to patient care changes the process. It improves physical and psychological well-being. The InterStellar framework focuses on patient safety. It shows that a holistic quality improvement model greatly reduces mortality rates. It also raises the quality of care in hemodialysis settings (Palencia H et al., 2025). The extended care model for breast cancer patients also proves the value of this method. Holistic nursing lowers anxiety and depression. This helps patients manage themselves and improves their quality of life (Liang W et al., 2025). These findings show that holistic nursing tracks more than just standard medical numbers. It builds a compassionate connection between healthcare providers and patients. Adopting a holistic nursing philosophy leads to complete care. It meets the needs of the whole person. This fulfills the essence of providing care from
Additional Blogs
The Art of Holistic Nursing: Access here
Additional Resources
“How Holistic Medicine Complements Modern Science” (2025). Science News Today. Access here
Wisner, W. (2025). “Understanding Holistic Health: Types and Benefits”. Health. Access here
“The Benefits of Holistic Medicine: Supporting Mind, Body, and Spirit”. (2025). AANMC. Access here
Marks, H. (2025). “What Is Holistic Medicine and How Does It Work?”. WebMed. Access here


















 Written by Nadine Westwood
Written by Nadine Westwood


 Written by Pat Lee.
Written by Pat Lee.