By – James M. Katz, BA
Most of us know those moments when standard health advice falls short. One expert talks about diet alone. Another focuses on exercise. A third emphasizes meditation. This leaves us confused about putting all the pieces together. A comprehensive approach to holistic wellness provides the answer. Research and practice over the last several years have shown that true well-being doesn’t fix isolated issues. The human body works as an interconnected system. Physical health, mental clarity, emotional balance, and spiritual well-being are the foundations of one complete system. This piece explains how a comprehensive approach to holistic wellness can revolutionize your life. The core principles and practical strategies will help you build a tailored path to complete well-being that enhances every aspect of your health.
Understanding the Holistic Wellness Revolution
The comprehensive wellness movement has brought remarkable changes to our approach toward holistic healthcare and wellbeing. The global wellness economy has grown substantially from $3.70 trillion in 2015 to $4.20 trillion in 2017, showing our collective move toward detailed health solutions.
The Rise of Wellness Thinking
Modern understanding of comprehensive holistic wellness has deep roots in ancient civilizations like Greece, Rome, and Asia. These cultures developed advanced ways to maintain health. Ancient practices, especially Traditional Chinese Medicine and Ayurveda, focused on creating balance between body, mind, and spirit. Modern research and understanding have now revived these time-tested principles.
Why Traditional Approaches Fall Short
Traditional wellness approaches don’t work well because they:
• Treat symptoms instead of addressing root causes
• Don’t consider environmental effects on health
• Create solutions without scientific evidence
Traditional programs typically achieve nowhere near 30% employee participation. This shows we need a more detailed approach. The biggest problem isn’t just about participation. These approaches don’t deal very well with individual needs because they use a one-size-fits-all strategy.
The Integration of Mind, Body, and Spirit
Better health comes from balancing physical, mental, emotional, and spiritual dimensions. Research supports this idea. When we address these connected aspects together, we create lasting health outcomes.
Recent studies show 81% of people now prioritize physical health, while 74% focus on mental health, and 71% emphasize emotional wellbeing. These numbers reflect our growing awareness that wellness isn’t separate – it’s a dynamic mix of life’s various aspects.
The power of comprehensive wellness lies in recognizing the mind-body connection. Mental and emotional states substantially affect our physical health, and vice versa. This connected approach creates a foundation for lasting wellness that covers every aspect of our being.
The Five Pillars of Holistic Healthcare Transformation
The path to comprehensive wellness rests on three fundamental pillars that work in perfect harmony. These pillars create the foundations for lasting change in our lives.
Physical Vitality and Movement
Physical well-being is the life-blood of comprehensive wellness. Regular movement improves not just physical health but also affects our vitality. This vitality determines our health, happiness, positive relationships, and life satisfaction. Physical activity builds strength and creates a foundation for overall wellness.
Here are the key benefits of physical vitality:
• Improved cardiovascular health and lung function
• Higher energy levels and reduced fatigue
• Better sleep quality and deeper rest
• Reduced risk of chronic diseases
Mental Clarity and Emotional Balance
Mental holistic wellness extends way beyond the reach and influence of stress management. Recent studies show that comprehensive approaches to mental health can substantially affect our overall well-being. Spiritual practices and mindfulness help people cope with stress, anxiety, and depression.
The sort of thing i love is how our emotional and mental states interconnect. Dr. Gabor Mate’s research emphasizes that “safety is not the absence of threat; it is the presence of connection”. This understanding has transformed our approach to mental wellness.
Spiritual Connection and Purpose
Spiritual wellness brings the most profound changes in our transformation. Spiritual wellness isn’t about religion – it gives meaning to life and helps understand our purpose.
Dr. Lisa J. Miller’s neuroscience research shows how spirituality relates to a more resilient and reliable brain. On top of that, Dr. Bruce Lipton’s foundational research in energetics and epigenetics shows how our thoughts affect our DNA. This suggests that spiritual practices cultivating compassion, peace, and love can activate gene expression. The result is a physically healthier and more joyful life.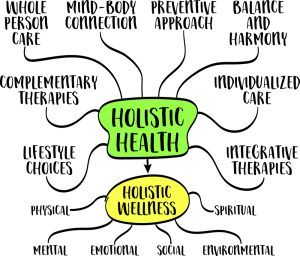
The human spirit needs purposeful practice just like our bodies need exercise. A nurtured spirit develops resilience to experience peace and purpose during life’s most challenging moments. This spiritual strength becomes our anchor and helps us direct through difficulties with grace while we retain our sense of purpose even in adversity.
Creating Your Holistic Wellness Foundation
A strong foundation for an all-encompassing approach to wellness begins with understanding our current position. Let’s discover how we can build a framework for lasting change through careful planning, setting goals, and daily habits.
Assessing Your Current Wellness State
The first step in this experience requires us to assess our current state using reliable tools. Research shows that the most trusted instruments include the Wellness Evaluation of Lifestyle, Five-factor Wellness Evaluation, and the Body-Mind-Spirit Wellness Behavior Inventory. These detailed tools help us get into several aspects of our wellbeing:
• Physical vitality and health patterns
• Mental and emotional balance
• Social connections and support systems
• Purpose and spiritual direction
• Environmental influences
Setting Integrated Holistic Wellness Goals
A full picture of our current state allows us to create meaningful goals. Studies show that using standardized wellness measurement instruments in primary care settings can boost preventive services and behavioral health outcomes by a lot. Note that wellness extends beyond the absence of illness – it’s a lifelong process where we make decisions to live a more balanced and meaningful life.
We can make our wellness experience more manageable by creating SMART goals (Specific, Measurable, Achievable, Relevant, and Time-bound). This structure will give a clear path for our wellness transformation.
Building Daily Wellness Rituals
Daily practices hold the real power of transformation. Research shows that intentional everyday rituals can turn ordinary routines into moments of personal significance and reflection. These rituals need three basic elements: intention, attention, and repetition.
Here are five foundational rituals that can boost our overall wellness:
1. Morning Meditation: Start each day with grounding practices to reduce stress and improve concentration
2. Mindful Movement: Add regular physical activity that lines up with our energy levels
3. Nature Connection: Time outdoors clears our mind and improves our mood
4. Evening Reflection: Practice gratitude and review our daily experiences
5. Digital Detox: Stay away from devices at least an hour before bed to improve sleep quality
These rituals, when practiced consistently, can boost our self-worth and create inner peace. Note that wellness means something different to each person, and what helps one person might not help another. Success comes from building a foundation that strikes a chord with our personal needs while staying flexible enough for growth and adjustment.
Navigating Common Transformation Challenges
Living a holistic wellness lifestyle brings its own set of challenges. Learning to guide ourselves through these obstacles makes our experience smoother and environmentally responsible. Let’s explore ways to overcome these common hurdles together.
Overcoming Resistance to Change
Our minds often resist change when we start our wellness experience. Research shows that resistance isn’t just about willpower – it’s deeply rooted in our brain’s hardwiring to keep us safe and maintain familiar patterns. This understanding helps us approach change with more compassion and patience.
Our brain learns to survive through familiar patterns. Rather than fighting this resistance, we can work with it by setting SMART goals that arrange with our brain’s natural tendencies. This approach creates lasting change without triggering our internal defense mechanisms.
Managing Time and Energy
Managing energy, not just time, plays a vital role in holistic transformation. Research indicates that while time is finite, energy can be systematically expanded and renewed through specific rituals. This change in viewpoint has revolutionized our daily wellness practices.
Our bodies operate in natural cycles called ultradian rhythms, consisting of 90-120 minute periods of high energy followed by lower energy phases. Understanding these rhythms helps optimize our daily activities:
• Schedule challenging tasks during high-energy periods
• Take strategic breaks during natural energy dips
• Practice deep breathing exercises between activities
• Create boundaries around technology use
• Arrange activities with our natural energy flows
Maintaining Motivation and Momentum
Motivation needs more than willpower. Studies show that emotional connections to wellness goals create more sustainable change. The process matters more than the end result for maintaining long-term momentum.
The 1% Better Approach works effectively. Small, incremental improvements work better than dramatic changes. A person who exercises for 10 minutes today aims for 11 minutes tomorrow. This compound effect creates sustainable progress without system overwhelm.
Emotional energy management plays a key role in maintaining momentum. Research shows that positive situation reframing and expressing appreciation build emotional resilience for long-term transformation. Brief but regular breaks throughout the day help recharge and maintain steady progress toward wellness goals.
Strategic solutions and understanding these challenges create a more sustainable approach to our wellness experience. Note that transformation isn’t about perfection – it focuses on progress and consistency in daily choices.
Measuring Your Holistic Wellness Progress
Wellness tracking needs both art and science to work well. Research and practice show that measuring wellness means more than just counting steps or tracking calories.
Key Wellness Indicators to Track
The CDC uses various surveys to assess health and wellness in multiple ways. Here are the essential indicators you should track:
• Physical Health Metrics: Daily activity levels, sleep quality, and vital signs
• Mental Wellness Markers: Stress levels, anxiety patterns, and mood fluctuations
• Emotional Balance: Social connections and relationship quality
• Spiritual Growth: Sense of purpose and inner peace
• Environmental Impact: Living space wellness and community involvement
Studies show that several factors affect our mental and emotional health. These include worry, mood, sleep, stress, relationships, and alcohol consumption. Monitoring these connected elements creates a better picture of overall wellness.
Using Technology for Wellness Monitoring
Technology makes tracking wellness easier than ever. Smart watches and fitness trackers have become essential tools. More than 300 million people used wellness apps in 2023. These devices track everything from physical activity to sleep patterns and give great insights about overall wellbeing.
A remarkable fact is that 80% of wearable device users want to share their health information with healthcare providers. This blend of technology and professional healthcare support creates an all-encompassing approach to wellness monitoring.
Adjusting Your Approach Based on Results
Analytical insights help guide decisions and make meaningful changes. The CDC’s behavioral risk factor surveillance system helps understand how many days mental or physical health might not be optimal. This data helps develop activities, programs, and policies that improve overall health.
You should look at multiple data points when checking progress:
1. Short-term Indicators: Daily energy levels, mood patterns, and physical activity
2. Medium-term Trends: Monthly sleep quality, stress management effectiveness
3. Long-term Progress: Quarterly wellness assessments, yearly health markers
Studies show that standardized wellness measurement tools substantially improve preventive services and behavioral health outcomes. The Warwick-Edinburgh Mental Wellbeing Scale works well to monitor mental wellbeing in the general population. This helps people make better decisions about their wellness.
Note that measuring progress isn’t about being perfect. It helps you understand patterns and make smart adjustments. Modern technology combined with traditional wellness metrics creates a more nuanced and effective way to track your wellness experience.
Building a Sustainable Wellness Lifestyle
The path to lasting wellness starts when we shape our environment to support our health goals. Research shows that creating safe and supportive environments leads to better health outcomes and improves overall wellbeing.
Creating Supportive Environments
Our environment plays a significant role in our wellness. Studies suggest that supportive spaces help reduce high-risk behaviors and mental health issues. Here’s how we can create a wellness-friendly space:
• Physical Space Organization: Declutter and arrange for optimal flow
• Natural Elements: Add plants and natural light
• Wellness Zones: Set up areas for meditation and exercise
• Digital Boundaries: Create tech-free spaces for peace of mind
• Air Quality: Keep proper ventilation and purification
Research shows that colleges with wellbeing resources and programs see better student outcomes. We can use these insights to improve our personal spaces and reach our wellness goals.
Developing Healthy Relationships
Our relationships shape our wellness deeply. Studies show that connecting with peers helps ease loneliness and builds a sense of belonging. Healthy relationships need several key elements to last.
People with strong social connections have better health outcomes. They show lower rates of anxiety and depression, higher self-esteem, and build more trusting and cooperative relationships.
Active listening and open communication help nurture these bonds. Research shows that emotional support helps mental health recovery, and small gestures can make a big difference.
Maintaining Long-term Balance
A sustainable wellness lifestyle focuses on progress, not perfection. Studies suggest that habits take about 66 days to form. This means we need patience and consistency.
Long-term balance needs attention to every aspect of wellness. Research shows that wellness changes constantly and needs good self-care. We should regularly check and adjust our approach based on our needs.
Strategic breaks throughout the day boost productivity and creativity. Our bodies work in 90-120 minute cycles of high and low energy. Planning activities around these natural cycles helps maintain balance.
Daily rituals support overall wellbeing effectively. Research suggests that workshops, seminars, and events help ease stress and provide ways to handle challenges. These opportunities become part of our routine, making wellness natural rather than another task.
This approach to wellness creates a lifestyle that lasts. Studies show that sustainable living means understanding how our choices affect the world and finding ways for everyone to live better. Our wellness practices benefit us, our community, and our environment.
Conclusion
All-encompassing wellness is more than just another health trend. It’s an approach that recognizes how our physical vitality, mental clarity, emotional balance, and spiritual wellbeing are interconnected. We’ve seen these elements work together to create positive changes that last.
Experience and research tell us that lasting change doesn’t need perfect execution or major life overhauls. The foundation for lasting wellness comes from small, consistent steps backed by daily mindful practices and tech-enabled tracking. We succeed by creating environments that help us grow, building supportive relationships, and staying flexible as we move forward.
Note that wellness isn’t a destination – it’s a continuous trip of growth and discovery. Every step toward better health brings us closer to the balanced, vibrant life we deserve. This could be through morning meditation, mindful movement, or meaningful connections. Our all-encompassing approach doesn’t just improve our health – it improves every aspect of our lives. These positive changes create ripples that spread way beyond ourselves.
If you’re part of the nursing field and are looking for a way to expand your healthcare career, then you should visit the American Institute of Health Care Professional’s online certification program in Holistic Healthcare. The certification program is designed to give you a greater understanding of the holistic wellness field. All of the required courses are based on competency exams and are taken 100% online. For a full review of the program as well as the required courses, please press here.
FAQs
Q1. What is holistic wellness and how does it differ from traditional approaches? Holistic wellness is an approach that considers the interconnectedness of physical, mental, emotional, and spiritual aspects of health. Unlike traditional approaches that often focus on treating isolated symptoms, holistic wellness aims to create harmony between all dimensions of well-being for overall health and life satisfaction.
Q2. How can I start incorporating holistic wellness practices into my daily routine? Begin by assessing your current wellness state and setting integrated goals. Implement daily rituals such as morning meditation, mindful movement, nature connection, evening reflection, and digital detox. Remember to start small and focus on consistency rather than perfection.
Q3. What are some common challenges in maintaining a holistic wellness lifestyle? Common challenges include overcoming resistance to change, managing time and energy effectively, and maintaining motivation. To address these, focus on setting SMART goals, aligning activities with your natural energy cycles, and adopting a ‘1% Better Approach’ for sustainable progress.
Q4. How can I measure my progress in holistic wellness? Track key wellness indicators across multiple dimensions, including physical health metrics, mental wellness markers, emotional balance, spiritual growth, and environmental impact. Utilize technology like wellness apps and wearable devices to monitor your progress, and regularly review and adjust your approach based on the results.
Q5. What role do relationships and environment play in holistic wellness? Supportive relationships and environments are crucial for sustainable holistic wellness. Focus on creating spaces that promote well-being, nurturing healthy connections with others, and maintaining a balance across all dimensions of wellness. Remember that wellness is an ongoing journey that involves continuous adaptation and growth.
Research Articles:
Rationing of nursing care, a deviation from holistic nursing: A systematic review. Lata Mandal MSc Nursing, Et Al. Nursing Philosophy Volume 21, Issue 1. Special Issue: Missed care, care left undone: Organisation ethics and the appropriate use of the nursing resource. January 2020 e12257
Full Article
Holistic Nursing in Practice: Mindfulness-Based Yoga as an Intervention to Manage Stress and Burnout. Hilcove K, Marceau C, Thekdi P, Larkey L, Brewer MA, Jones K. Journal of Holistic Nursing. 2021;39(1):29-42.
Full Article
Phenomenology for the Holistic Nurse Researcher: Underpinnings of Descriptive and Interpretive Traditions. Patton CM. Journal of Holistic Nursing. 2020;38(3):278-286.
Full Article
Implementing a Spiritual Care Subject for Holistic Nursing Practice: A Mixed Method Study. Cooper KL, Chang E. Journal of Holistic Nursing. 2023;41(3):233-245.
Full Article






 Written by
Written by  By Lucy Peters,
By Lucy Peters,




 Written by Charles Schubert.
Written by Charles Schubert.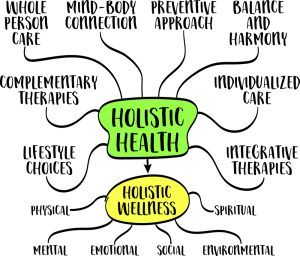





 Written by Charles Schubert
Written by Charles Schubert