Abuse has many faces. It can be physical, it can be sexual and it also can be emotional. Prolonged emotional abuse which is chronic overtime chips away at the person and places him or her into a state of constant survival. Instead of stress responses acting as responses in the moment to survive, they become a constant state of existence. This is one of the primary differences between PTSD and C-PTSD. Under long periods of repeated duress due to emotional abuse or even neglect, the brain rewires itself to exist within a survival state. With no acute emotional wound but a collection and series of events, emotional abuse or any type of abuse that is chronic or repeated, becomes difficult to discern what started ignition from survival response to survival state itself. The delicate balance of allstasis or the ability to remain stable adjusts to constant change eventually reaches a state of allostatic load that eventually can crash in which the survival state becomes a new state that overtakes the person.
Please also review AIHCP’s Trauma Informed Care Program as well as AIHCP’s numerous behavioral healthcare certifications
Neglect and Emotional Abuse
Emotional abuse is a trauma overtime that can lead to a survival state due to the repeated abuse or neglect. Around 80 percent of all maltreatment of children can be reduced to emotional abuse and neglect. While these things do not necessarily require physical or sexual abuse, they gradually wear the person down. This is especially true of children with developing brains that can be hindered by chronic emotional abuse or neglect.
According to Contreras, neglect as a type of abuse categorized as omission (2024, p. 183). With neglect and emotional abuse, the child or even person enters into a state of survival mode. One is on red alert constantly for what may go wrong in a particular day due neglect or emotional abuse. When those limits are met, just like any stress, the person is able to adjust or lose ability to cope and falls victim to the stressor, trauma or abuse. These individuals will have emotional regulation issues, hyper or hypo arousal states, and react to the abuse in different ways according to these states. Individuals under constant barrage can fall into fight, flight, fawn or fade as the daily barrage of abuse or neglect degrades their personhood, identity and mood. In these cases to survive the prolonged neglect and abuse, the person appeases, becomes aggressive with others, looks to escape confrontations, look to please, or fade into thinking there is no true abuse (Contreras, 2014, p. 201-202). From this, neglect and emotional abuse drains the person of self, identity and self worth, replacing daily actions into survival responses adapted for prolonged exposure to the stressors or minor traumas of the day. It is because of this that many who have gone through such abuse or neglect, develop C-PTSD.
Emotional Abuse and Neglect
Neglect to basic needs, both physical and mental are detrimental to children and their development into mentally stable adults. Neglect and emotional abuse not only hurts the development of the brain but also can lead to physical ailments due to the constant state of survival.
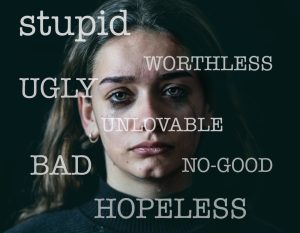
Chronic emotional abuse according to Contreras is any words or non physical actions that hurt, belittle, weaken, manipulate or frightens a person. In addition the abuse causes distortion and confusion that shakes the person’s very stability in life. Many forms of mental abuse are carried on through neglect, but also intimidation, manipulation, objectification, gaslighting, yelling, and even obsessive jealousy (2024, p. 184). Individuals are left with exhaustion, depression, low self esteem, and feel trapped. In doing so they look for maladaptive ways to cope with trauma. Many times, especially children, but also adults, can become stuck in a co-dependent relationship which are detrimental to all levels of their existence. While the person is not in a life or death situation, the person does develop a shattered sense of self. This is accomplished through mind games, devaluation, and scheming that mentally undermines the person. Contreras lists manipulation, gaslighting and objectification as key ways of controlling and harming the person (2024, p. 187-189).

Manipulation
Contreras defines manipulation as a type of subtle abuse to debilitate a person’s will and capabilities to obtain personal gain, control, submission, obedience and pleasure from the abused (2024, p. 187). Individuals who are constantly manipulated lose sense of self, and self esteem leading them to feel used, depressed and hopeless. If they do not respond to the manipulation, many emotionally and neglected fear abandonment and rejection from the abuser.
Gaslighting
According to Contreras, gaslighting is an effective for abusers to control and manipulate their victim. They do so by making the individual doubt his or her own reality making the person feel crazy or insecure (2024, p. 188). It intentional to control the person and keep them within the abuser’s web of chaos.
Objectifying
In many cases, those who are emotionally abused, as well as physical, are objectified as property. The person loses autonomy of self. Contreras lists a variety of ways objectification occurs. Instrumentality refers to using the person as a tool to meet an end or satisfy one’s own goals. Denial of autonomy refers to the inability for the person to act on his or her own without consent from the abuser. Ownership refers to a person’s literal autonomy belonging to the abuser to be used and sold as the abuser sees fit. Denial of subjectivity dismisses the abused and his or her experiences or feelings as not worthy of attention or need. Finally silencing refers to taking away the person’s voice (Contreras, 2024, p. 190-191).
Individuals who objectify other human beings in general lack any form of empathy, are ego-centric, and put their needs and goals over everyone. They are usually tied to the personality disorder of narcissism (Contreras, 2024, p. 189).
Unfortunately, this leads to trauma bonding which according to Contreras, leads the abused to an attachment with the abuser that disempowers the individual into a perpetual state of defeat under the mirage of being loved (2024, p. 192).
Conclusion

Severe neglect, as well as emotional abuse is a different wound than physical wounds. They may not inflict immediate death or harm but they lead to a chronic breaking of the spirit and the person’s development. It leads to a host of emotional and mental problems that destroy the mind and soul. Due to its usual chronic state and repeated offenses, it wears the person down and can manifest in states of C–PTSD where the person enters into a constant survival state that breaks down not only the mind but the body. It steals the joy of life and the dreams of others.
Please also review AIHCP’s Trauma Informed Care Certification as well as AIHCP’s Healthcare Certifications
Additional Blog
PTSD vs C-PTSD. Click here
Resource
Contreras, A. (2024). Traumatization and Its Aftermath: A Systematic Approach to Understanding and Treating Trauma Disorders”
Additional Resources
Valdez, R. (2025). “Signs of Emotional Abuse”. VeryWellMind. Access here
Pietrangelo, A. & Raypole, C. (2025). “How to Recognize the Signs of Emotional Abuse”. Healthline. Access here
“Emotional Abuse”. Psychology Today. Access here
“What Is Emotional Abuse”. National Domestic Violence Hotline. Access here




















