Written by Veronica Turner.
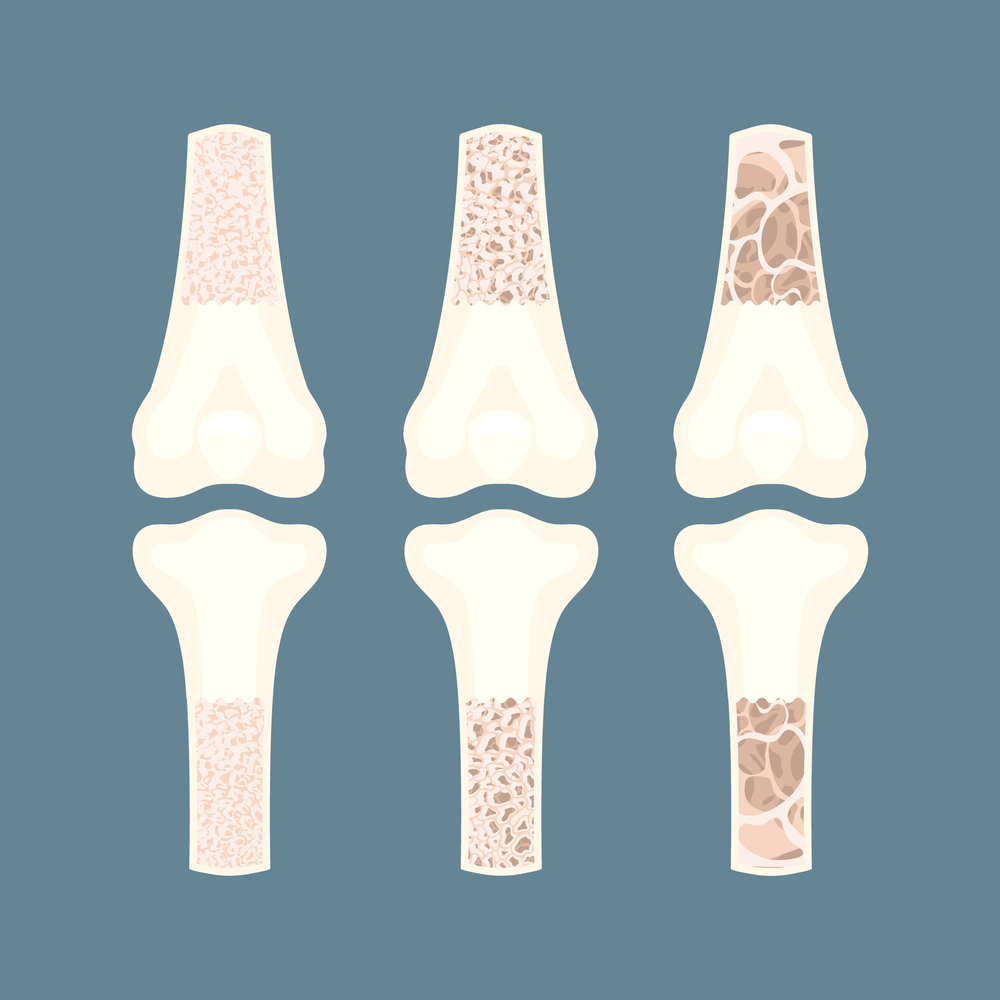
In the US alone, around 10 million people suffer from osteoporosis, while another 44 million are on the path to becoming affected because of low bone density. The thing about osteoporosis is that, more often than not, patients don’t know they are at risk until a simple fall turns into something serious.
While a complete reversal of the damages caused by osteoporosis is not possible, specialists can help patients slow down the progression and improve bone density through a holistic approach that combines medication, nutrition, lifestyle changes, and innovative therapies.
Experts see promise in this approach, and ongoing advancements are shaping the landscape of orthopedic care across the US.
In today’s piece, we will examine the most common practices used to prevent and slow down the progression of osteoporosis before it becomes a life-altering health problem.
Who Is at Risk of Developing Osteoporosis?
Osteoporosis doesn’t discriminate, but certain factors heighten the risk. Age is a primary contributor since bone density starts to decline naturally in the mid-30s and accelerates after age 50.
Women are more susceptible to losing bone density due to the changes associated with menopause, which comes with reduced estrogen levels. Among its many jobs in a woman’s body, estrogen is also responsible for maintaining bone mass.
Genetics play their part, too. If osteoporosis runs in the patient’s family, they may also have a predisposition to loss of bone density and easy fractures. Additionally, ethnicity matters – studies show that Caucasian and Asian populations tend to have a greater incidence compared to others.
However, age, sex, and genetics are not the only factors that determine whether osteoporosis will impact a person’s quality of life.
Lifestyle choices also tip the scale. Low calcium intake throughout life contributes significantly to bone strength over time. Also, people with a sedentary lifestyle have weaker bones due to a lack of consistent physical activity.
Our bones, like muscles, strengthen when subjected to stress. This is why specialists recommend weight-bearing exercises such as walking, running, or resistance training as forms of prevention.
Lastly, patients who are on long-term medication are also at a higher risk since steroids or specific anticonvulsants may diminish bone density with prolonged usage.
This is why medication alone is not enough to help patients who are already suffering from osteoporosis or those who are at higher risk. We need a more holistic approach to understanding bone health in order to help patients live longer, happier lives.
The Role of Nutrition in Bone Health: Beyond Calcium
A well-balanced diet rich in diverse nutrients that promote bone health is pivotal in managing low bone density. Patients need calcium, vitamin D, magnesium, and Omega-3 fatty acids to maintain and improve their bone health.
Foods like fatty fish (salmon or mackerel), egg yolks, chia seeds, flax seeds, and fortified milk are excellent sources of calcium and Omega-3. Also, a daily dose of sunlight helps the body produce vitamin D, which is needed to enhance calcium absorption.
For magnesium (needed for bone mineralization), patients must incorporate nuts like almonds or cashews, whole grains such as brown rice, and leafy greens.
Healthy bones also need protein since they form the structural foundation. Therefore, a healthy diet must include lean meats, tofu, beans, and other protein sources.
Most healthcare scientists and specialists agree that a well-balanced diet rich in healthy nutrients is also great for preventing bone mass loss and osteoporosis. Balanced meals with ample vegetables and fruits alongside lean proteins and cutting down on processed foods high in sodium or sugar are the best ways to maintain optimal strength throughout life!
The Connection Between Gut Health and Strong Bones
Gut health affects how nutrients like calcium and vitamin D get absorbed into the bloodstream, directly influencing bone strength.
Also, chronic inflammation due to poor gut health can accelerate bone loss. An inflamed intestine might not absorb nutrients effectively, depriving bones of essential building blocks.
Emerging studies suggest that specific gut-derived molecules play roles in signaling pathways crucial for bone remodeling. So, by maintaining a balanced diet rich in fiber and probiotics, patients can nurture both their digestive system and skeletal health.
Keeping an eye on gastrointestinal wellness helps fortify bones against osteoporosis over time!
Impact of Lifestyle Adjustments on Osteoporosis
Lifestyle choices hold significant sway over bone health, and the good news is that it’s never too late to make improvements.
While prevention is usually the best approach, individuals can still make positive lifestyle changes that can lead to stronger bones and a reduced risk of fractures.
Take smoking cessation as an example. Smoking accelerates bone loss by affecting blood flow to bones, hindering calcium absorption. Quitting helps reverse these effects, allowing the body to have better access to essential nutrients for bone maintenance.
Alcohol moderation also contributes positively. Excessive alcohol intake weakens bones and disrupts balance, increasing fall risks. Cutting back not only strengthens skeletal structure but also improves overall well-being.
Incorporating regular physical activity into one’s daily routine is also a significant positive change. However, if patients already suffer from low bone density or have had previous fractures due to osteoporosis, it can be difficult to suddenly start being more active.
This is where local resources, such as specialized clinics, can make a huge difference. The regional aspect is essential because someone who lives in Alabama and suffers from mobility issues can’t take the train, car, or plane to find a specialist in New York. They need access to well-trained orthopedic physicians in Alabama so they can work on their mobility on a day-to-day basis.
Orthopedic physicians provide guidance on integrating exercise safely into routines tailored to individual needs, whether through physiotherapy sessions or community-based fitness programs focused on weight-bearing exercises like walking or light strength training.
Complementary Therapies to Consider
Complementary therapies emerged from a mix of traditional practices and modern research. While not all these practices enjoy scientific backing, many patients find pain relief and support within these therapies.
Therefore, integrating these methods into traditional treatment plans can improve overall well-being and support bone health. However, it’s essential for patients to consult a healthcare professional before giving any of these therapies a go.
With that being said, here are some of the most well-known and lauded complementary therapies that are often included in the holistic health approach of osteoporosis management.
Acupuncture
Acupuncture is an ancient practice that targets specific points to alleviate pain associated with osteoporosis. It is believed the practice stimulates the body’s natural healing processes, which helps reduce inflammation and discomfort without medication reliance. Many patients find this approach soothing and beneficial for managing chronic pain.
While some specialists are not too convinced by this practice, there are studies that show acupuncture can reduce chronic pain, like the one associated with osteoporosis. Although mechanisms are still debated among scientists, positive results encourage further exploration.
Tai Chi and Yoga
These two ancient practices have received recognition through studies demonstrating improved balance and physical function in older adults.
Yoga fosters strength while promoting flexibility through mindful movement patterns. Regular practice encourages proper alignment, which can also ease strain on joints affected by low bone mass.
Tai Chi combines gentle movements with focused breathing, significantly improving balance. This mind-body exercise reduces fall risks by enhancing coordination, a vital benefit since falls pose a significant threat to those with weakened bones.
Exploring the Use of Herbal Supplements
Herbal supplements, like red clover, offer potential advantages in maintaining bone density postmenopausal due to their phytoestrogen content. However, patients should consult their healthcare providers before adding these supplements to their regimen.
While studies have examined the effects of phytoestrogens on bone density postmenopausal, the evidence remains mixed. Plus, daily red clover consumption may interact with medication, which is why medical advice is needed.
Chiropractic Care and Its Impact on Posture Alignment
Though controversial at times, chiropractic care is well-regarded by many patients.
Chiropractors address misalignments that could worsen over time due to osteoporosis-related complications such as spinal curvature changes or old fractures that may impact posture maintenance.
Adjustments help realign vertebrae, ensuring better weight distribution across the entire frame and reducing unnecessary stressors.
Stress Reduction Techniques and Their Influence on Bone Health
Stress plays a significant role in overall health, impacting even bone density. Chronic stress releases cortisol, a hormone that, when elevated over time, can lead to decreased calcium absorption and increased bone loss.
Therefore, stress reduction techniques, like mindfulness or deep breathing exercises, can mitigate these effects and positively influence bone health.
Mindfulness meditation encourages relaxation and fosters resilience against daily stresses. Regular mindfulness practice has been shown to lower cortisol levels, contributing indirectly to better calcium metabolism.
Deep breathing exercises also help combat stress’s physiological impacts. They activate the parasympathetic nervous system, which counteracts the body’s “fight or flight” response triggered during stressful times. Regular practice aids in maintaining hormonal balance, which is essential for healthy bones.
Additionally, engaging in hobbies or activities like art therapy provides emotional outlets. These pursuits promote mental well-being while distracting from anxieties that might otherwise contribute negatively to osteoporosis management efforts.
In Summary
Embracing comprehensive care ensures long-term bone health. Combining traditional treatments with holistic approaches like nutrition, exercise, and complementary therapies fosters a supportive environment for bone strength.
In summary, staying informed on advancements and personalized strategies helps healthcare providers guide patients toward healthier, more resilient bones for years to come.
Author Bio: Veronica Turner is a health and lifestyle writer with over 10 years of experience. She creates compelling content on nutrition, fitness, mental health, and overall wellness.
References:
Ji, M. X., & Yu, Q. (2015). Primary osteoporosis in postmenopausal women. Chronic diseases and translational medicine, 1(1), 9–13. https://doi.org/10.1016/j.cdtm.2015.02.006
Kelly, R. R., McDonald, L. T., Jensen, N. R., Sidles, S. J., & LaRue, A. C. (2019). Impacts of psychological stress on osteoporosis: Clinical implications and treatment interactions. Frontiers in psychiatry, 10, 200. https://doi.org/10.3389/fpsyt.2019.00200
Noel, S. E., Santos, M. P., & Wright, N. C. (2021). Racial and ethnic disparities in bone health and outcomes in the United States. Journal of bone and mineral research: the official journal of the American Society for Bone and Mineral Research, 36(10), 1881–1905. https://doi.org/10.1002/jbmr.4417
Vickers, A. J., Vertosick, E. A., Lewith, G., MacPherson, H., Foster, N. E., Sherman, K. J., Irnich, D., Witt, C. M., Linde, K., & Acupuncture Trialists’ Collaboration (2018). Acupuncture for chronic pain: Update of an individual patient data meta-analysis. The journal of pain, 19(5), 455–474. https://doi.org/10.1016/j.jpain.2017.11.005
Zhong, X., Zhang, F., Yin, X., Cao, H., Wang, X., Liu, D., Chen, J., & Chen, X. (2021). Bone homeostasis and gut microbial-dependent signaling pathways. Journal of microbiology and biotechnology, 31(6), 765–774. https://doi.org/10.4014/jmb.2104.04016
Please also review AIHCP’s Holistic Nursing Certification program and see if it meets your academic and professional goals. These programs are online and independent study and open to qualified professionals seeking a four year certification
