 Written by Yusuf Shaikh,
Written by Yusuf Shaikh,
Introduction
Sudden cardiac arrest (SCA) remains one of the leading causes of death worldwide. According to the American Heart Association (AHA), survival rates remain dismally low, particularly in out-of-hospital cardiac arrests (Benjamin et al., 2019).
While high-quality chest compressions and early defibrillation are foundational, recent studies reveal that structured teamwork and role delegation significantly increase return of spontaneous circulation (ROSC) and survival-to-discharge rates (Chan et al., 2021). High-performance resuscitation teams (HPRTs) aim to address these gaps by leveraging coordination, leadership, and practice.
The Limitations of Individual CPR
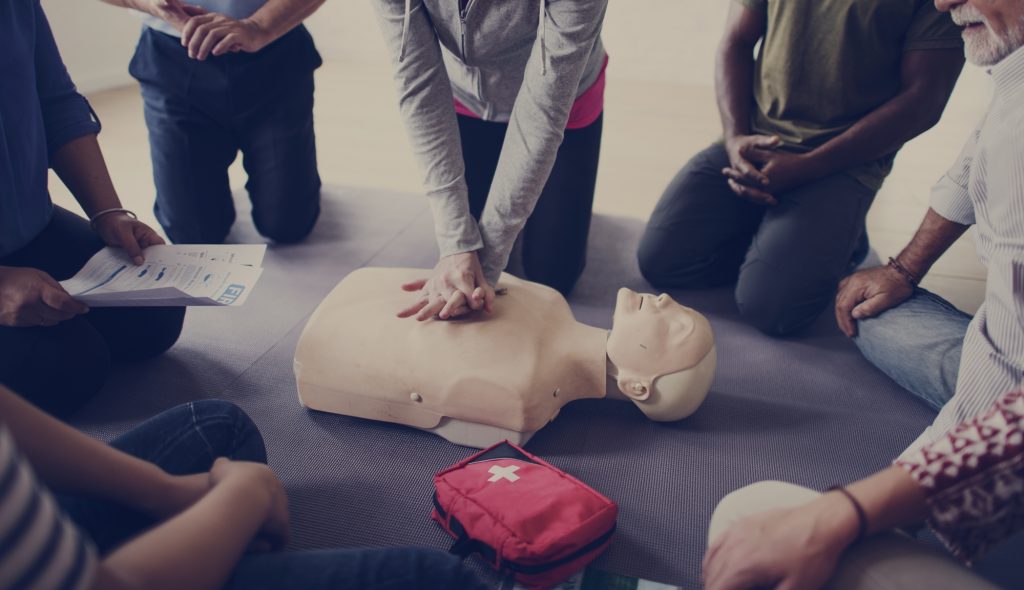
Traditional CPR training typically focuses on individual competency in basic life support (BLS). These programs are invaluable for equipping people with life-saving skills like chest compressions, rescue breaths, and the use of automated external defibrillators (AEDs). However, in actual emergency situations—especially in clinical or high-stress environments—CPR rarely occurs in isolation. More often, multiple team members are present, and unfortunately, their actions can become uncoordinated or inefficient without clear leadership or structured roles.
For example, if one person is compressing the chest while another is attempting to prepare an airway, the lack of communication can lead to pauses in compressions or ineffective ventilation. Even minor delays—just a few seconds—can dramatically reduce the chances of survival, particularly in cardiac arrest cases where every moment counts. Studies have shown that poor team coordination leads to lower quality chest compressions, missed shock opportunities, and slower administration of life-saving medications.
This is where individual CPR training falls short. It teaches what to do, but not how to do it in a team context under pressure. In high-acuity settings like hospitals, ambulances, or even large public gatherings, the need for synchronized efforts and designated roles becomes critical. Without that, even the most well-intentioned efforts may fall flat.
What Is a High-Performance Resuscitation Team?
An HPRT is a group of healthcare or trained lay responders who work together using pre-defined roles and a shared mental model during cardiac arrest situations. This approach optimizes every second of the “code” process. Common roles include:
- Compressor (performs high-quality chest compressions)
- Defibrillator (operates AED or manual defibrillator)
- Airway Manager (manages ventilation and oxygenation)
- Recorder (tracks time intervals and medications)
- Team Leader (coordinates actions and ensures protocol adherence)
Teams often follow structured debriefings and simulations to refine performance and reduce human error (Panchal et al., 2020).
Benefits of High-Performance Resuscitation Teams
1. Improved Patient Outcomes
Several studies show that hospitals implementing HPRTs see a significant increase in ROSC and neurologically intact survival (Abella et al., 2005). Pre-assigned roles reduce confusion and downtime between interventions.
2. Reduced No-Flow Time
No-flow time—the period when no chest compressions are delivered—has a direct correlation with poor outcomes. HPRTs drastically reduce this through seamless role transitions and real-time feedback tools (Bobrow et al., 2013).
3. Enhanced Communication
Clear, closed-loop communication is central to HPRTs. This minimizes misunderstandings and allows teams to act with confidence and precision under pressure.
4. Professional Development
Teams that train together build trust and psychological safety. These dynamics are essential not only for acute resuscitation but also for broader team effectiveness in high-stress medical environments (Weinstock et al., 2017).
Implementation Strategies
A. Regular Simulation Training
High-fidelity simulation labs allow teams to practice rare but critical events. The AHA recommends quarterly mock codes with post-event debriefings for maximum skill retention (AHA, 2020).
B. Role Standardization
Every team member should know their primary and backup roles. Color-coded vests, pocket cards, and standardized checklists can aid quick identification during a code.
C. Performance Metrics and Feedback
Objective data from CPR feedback devices (e.g., depth, rate, recoil) can be used in post-code analysis to identify strengths and areas for improvement.
D. Leadership Development
Strong team leadership correlates with better outcomes. Investing in leadership training for code team captains can help maintain order and morale in high-pressure situations (Knight et al., 2022).
Application in Non-Hospital Settings
High-performance team dynamics are not limited to hospitals. Fire departments, EMS units, and even large corporations with emergency response teams can benefit from this model.
Community organizations that conduct CPR drills with local EMS can drastically improve bystander CPR rates and SCA survival in public settings. Schools, airports, malls, and sports arenas are also adopting high-performance CPR strategies by training staff in team-based emergency protocols.
By implementing routine practice sessions and designated responder roles, these institutions can significantly reduce response time and improve coordination—ultimately saving lives in high-traffic environments where seconds count the most.
Future Outlook: AI and Smart Monitoring
AI-assisted feedback and predictive analytics tools are beginning to play a role in CPR training and performance assessment. Smart manikins, wearable monitors, and real-time coaching apps will likely play a larger role in shaping the next generation of HPRTs (Zhu et al., 2023).
Emerging technologies such as augmented reality (AR) overlays, automated error correction, and adaptive e-learning platforms are being piloted in leading hospitals and EMS academies.
These innovations promise to close the gap between training and real-world performance by providing continuous, personalized feedback that helps every team member—from novice to expert—improve their resuscitation technique.
Conclusion
CPR is no longer just a box to check in a training manual—it’s a dynamic, team-based response that can mean the difference between life and death. As healthcare becomes more complex and fast-paced, survival increasingly depends on how efficiently teams work together when every second counts. High-performance resuscitation teams don’t just know the steps; they practice them together, communicate clearly, and follow a structure that leaves no room for guesswork.
This kind of preparedness doesn’t happen by accident. It’s the result of targeted team training, simulated scenarios, and a culture that prioritizes communication and leadership under stress. Instead of relying on one person to carry the burden, responsibilities are shared and rotated with intention—from compressors to airway managers to medication administrators. Each role supports the other, creating a synergy that boosts overall performance.
Ultimately, patients deserve more than basic CPR—they deserve a well-orchestrated effort backed by training, trust, and timing. Investing in high-performance team resuscitation models not only improves survival outcomes but also strengthens the entire care ecosystem. Because when a crisis hits, it’s not about who knows CPR—it’s about how well the team performs together.
Author Bio
Yusuf Shaikh is a healthcare writer passionate about simplifying emergency response education. With a focus on CPR, first aid, and community safety, he contributes practical, research-driven content to platforms like CPRCare.com.
References
Abella, B. S., Alvarado, J. P., Myklebust, H., Edelson, D. P., Barry, A., O’Hearn, N.,.
American Heart Association (AHA). (2020). CPR & ECC Guidelines. Retrieved from https://www.heart.org
Benjamin, E. J., Muntner, P., Alonso, A., Bittencourt, M. S., Callaway, C. W
Chan, P. S., McNally, B., Tang, F., Kellermann, A., & CARES Surveillance Group. (2021). Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation: Cardiovascular Quality and Outcomes, 15(1), e007404.
Knight, L. J., Schilling, J., & Paul, P. (2022). Effective team leadership during resuscitation: A systematic review. Resuscitation Plus, 9, 100200.
Meaney, P. A., Bobrow, B. J., Mancini, M. E., Christenson, J., de Caen, A. R., Bhanji, F., … & Edelson, D. P. (2013).
Panchal, A. R., Berg, K. M., Kudenchuk, P. J., Del Rios, M., Hirsch, K. G
Please also review AIHCP’s Health Care Manager Certification program and see if it meets your academic and professional goals. These programs are online and independent study and open to qualified professionals seeking a four year certification
